|
Back to 2018 Program and Abstracts
PREDICTORS OF EARLY DISCHARGE AFTER PANCREATICODUODENECTOMY
Manuel Castillo-Angeles*1, Courtney E. Barrows1, Rodrigo Calvillo-Ortiz1, A. J. Moser1, Mark P. Callery1, Jennifer Tseng2, Tara S. Kent1
1General Surgery, Beth Israel Deaconess Medical Center, Boston, MA; 2Surgery, Boston Medical Center, Boston, MA
OBJECTIVE: Pancreaticoduodenectomy (PD) remains one of the most complex surgical procedures requiring prolonged hospital length of stay (LOS). Our aim was to identify predictors of early discharge after PD and to determine if these vary by operative approach.
METHODS: The ACS-NSQIP pancreas-targeted database was queried to identify patients who underwent pancreaticoduodenectomy (PD) in 2014-15. Patients with postoperative length of stay (LOS) ≤ 5 days were classified as early discharge. Multivariate logistic regression was used to identify predictors of early vs. late discharge. Subgroup analysis was performed to determine if predictors differ between open and minimally invasive (MIS) approach.
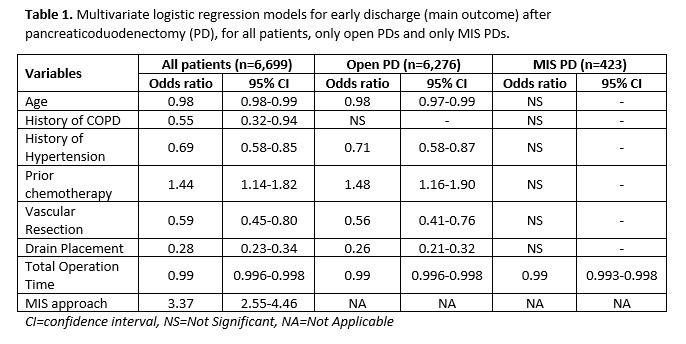
RESULTS: Of 6,699 PD patients, 602 (8.9%) were discharged early. Mean age was 64; 53.8% were male. 423 patients underwent an MIS approach (6.3%). Readmission rates were not significantly different between those who were discharged early and those who weren't (15.8% vs. 17.5%, respectively, p=0.373). Malignant pathology was also similar in both groups (79.1% vs. 80.9%, respectively, p=0.284). Younger age (p=0.004), absence of major comorbidities (COPD [p=0.032], hypertension [HTN, p<0.001]), prior chemotherapy (p=0.002), lack of vascular resection (p=0.001), absence of drains (p<0.001), MIS approach (p<0.001) and shorter operative duration (p<0.001) were independently associated with an early discharge. After subgroup analysis; younger age (p=0.001), absence of HTN (p=0.001), prior chemotherapy (p=0.002), lack of vascular resection (p<0.001), absence of drains (p<0.001) and shorter operative time (p<0.001) were significant predictors within the open PD group. However, within the MIS PD group, only shorter operative time was a significant predictor of early discharge (table 1).
CONCLUSION: Perioperative factors that predict early discharge after PD include younger age, absence of major comorbidities, neoadjuvant chemotherapy, MIS approach, lack of vascular resection, absence of drains and shorter operative time. Factors vary when patients were divided by operative approach. Total operative time was the only predictor that remained significant regardless of the approach. This information may be able to inform patient expectations, as well as postoperative efforts at recovery pace and disposition planning.
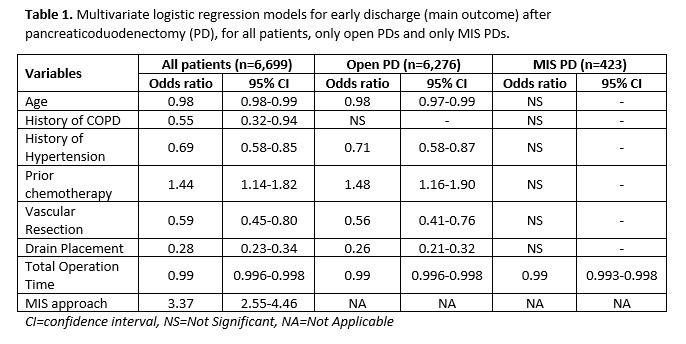
Table 1
Back to 2018 Program and Abstracts
|