|
 |
Back to 2018 Program and Abstracts
FLUID ADMINISTRATION AND SURGICAL OUTCOMES AFTER PANCREATODUODENECTOMY: EXTERNAL VALIDATION OF VARIABLE FLUID REGIMENES AT A TERTIARY REFERRAL CENTER
Marta Sandini*1, Carlos Fernandez-del Castillo1, Cristina R. Ferrone1, Katarina J Ruscic2, Matthias Eikermann1, Andrew L. Warshaw1, Keith D. Lillemoe1, Motaz Qadan1
1Department of Surgery, Massachusetts General Hospital, Boston, MA; 2Department of of Anesthesia, Critical Care, and Pain Medicine, Massachusetts General Hospital, Boston , MA
Background: Intraoperative fluid overload is associated with higher complication rates, prolonged hospitalization, and delayed recovery after major abdominal surgery. However, data following pancreatoduodenectomy (PD) are scarce and heterogeneous, with several proposed cutoffs for restrictive and liberal fluid infusion rates.
Aim: In a single cohort of PD patients from a tertiary referral center, we validated prior definitions of restrictive and liberal fluid regimens and analyzed whether they affected surgical outcomes.
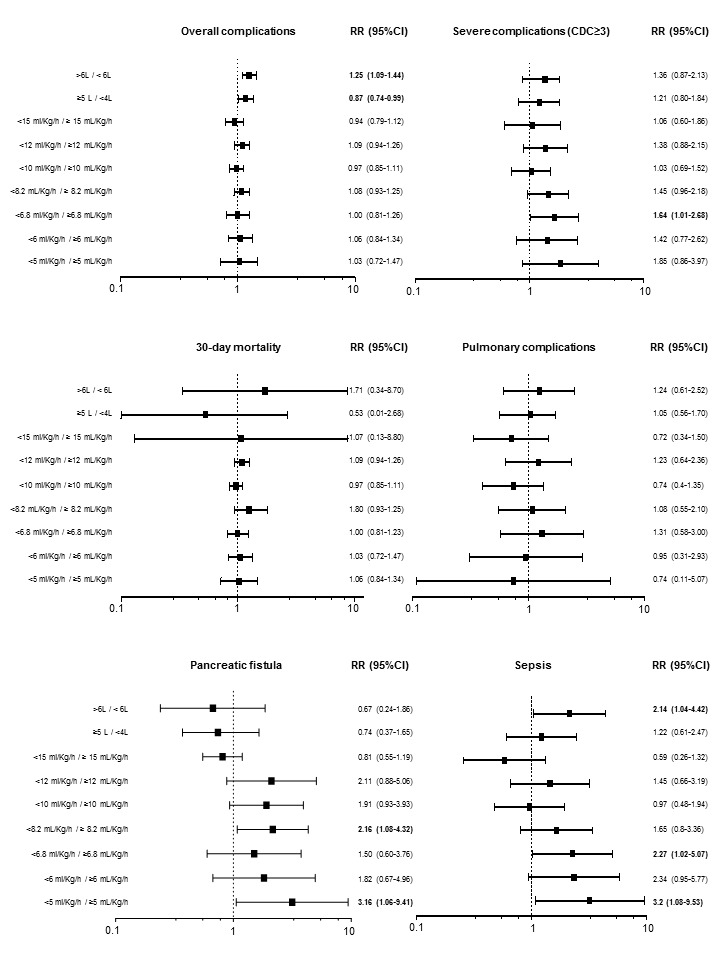
Methods: Studies comparing outcomes after pancreatic resections in patients who received standard vs. overload, restricted vs. overload, or restricted vs. standard intraoperative fluids were retrieved through web search. Anesthetic records of patients who underwent pancreatoduodenectomy at our institution were analyzed for intraoperative fluid administration, and surgical outcomes retrospectively analyzed from a prospective database. The relative risk (RR) and 95% confidence intervals for each outcome were calculated for the previously reported infusion regimens.
Results: Anesthetic data were available for 506 pancreatoduodenectomies. Mean age was 66±13 years, 45.8% were male, and mean BMI was 27.0±5.4. The median intraoperative fluid administration volume was 4250mL (3000-5500mL), with a median infusion rate of 10.2mL/kg/h (8.2-13.2mL/kg/h), and a 7:1 ratio of crystalloid to colloid administration. Nine cut-off values reported in previous studies were validated. Two regimens utilized total intraoperative volume cutoffs of <4000mL vs. >5000mL and <6000mL vs. >6000mL. The remaining 7 regimens evaluated various infusion rates, ranging from 5-15mL/kg/h.
Total volume administration of >6000mL and >5000mL were associated with an increased overall complication rate [RR 1.25 (1.09-1.44) and RR 1.17 (1.01-1.35), respectively], and >6000mL was associated with increased sepsis [RR 2.14 (1.04-4.42)]. Conversely, restrictive fluid regimens of <5mL/kg/h increased the risk of pancreatic fistula [RR 3.16 (1.06-9.41)] and sepsis [RR 3.20 (1.08-9.53)]; <6.8mL/kg/h was associated with an increased risk of major morbidity [RR 1.64 (1.01-2.68)] and sepsis [RR 2.27 (1.02-5.07)], while <8.2mL/kg/h was associated with an increased risk of pancreatic fistula [RR 2.16 (1.08-4.32)]. No fluid regimen-related effects were observed on pulmonary complications, surgical site infections, hospital length of stay, or mortality.
Conclusions: Variable restrictive and liberal intraoperative fluid infusion volumes and rates had limited effects on surgical outcomes following pancreatoduodenectomy, except at extreme restrictive and liberal values. Current recommendations for restrictive fluid administration and incorporation into enhanced recovery protocols require further validation following pancreatic resection, given the overall limited effect on morbidity and mortality.
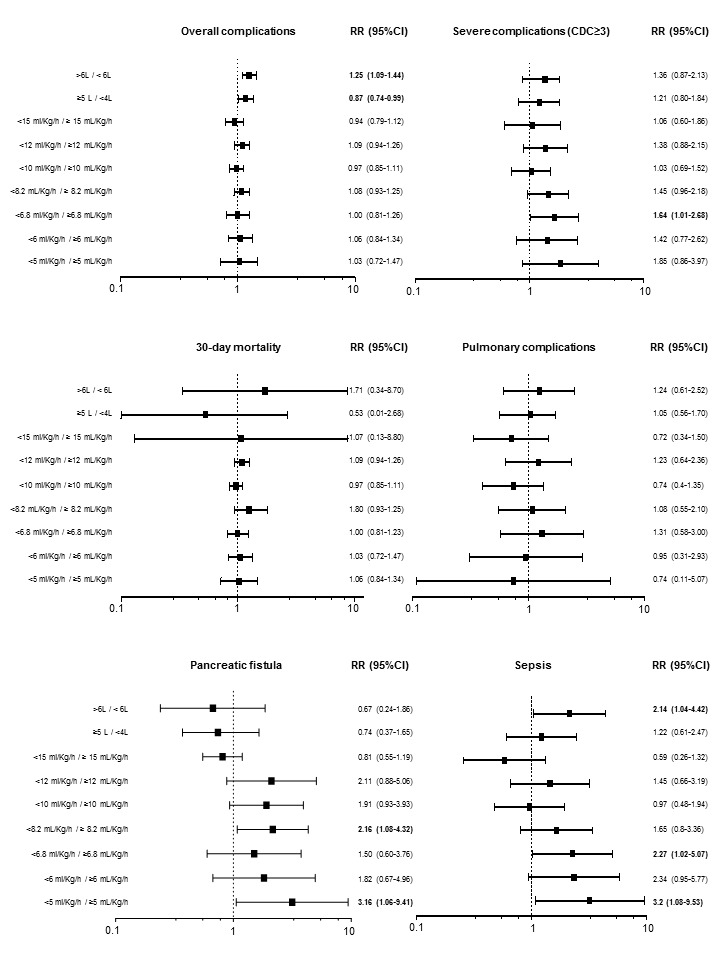
Effect of variable intraoperative fluid regimens on surgical outcomes after pancreatoduodenectomy.
Back to 2018 Program and Abstracts
|