|
 |
Back to 2018 Program and Abstracts
INTRA-ABDOMINAL SEPSIS FOLLOWING ILEOCOLIC RESECTION FOR CROHN's DISEASE: WHAT ARE THE RISK FACTORS AND ARE THEY CONSISTENT INTERNATIONALLY?
Amy L. Lightner*1, Nicholas P. McKenna2, Janindra Warusavitarne3, Antonino Spinelli4
1Colon and Rectal Surgery, Mayo Clinic, Rochester, MN; 2Surgery, Mayo Clinic, Rochester, MN; 3Colon and Rectal Surgery, St. Mark's Hospital and Academic Research Institute, London, United Kingdom; 4Colon and Rectal Surgery, Humanitas Research Hospital, Milan, Italy
Background: Two thirds of patients with Crohn's disease (CD) will require a major abdominal resection during their lifetime. The most common operation, ileocolic resection, can be complicated by postoperative intra-abdominal sepsis, leading to significant morbidity and risk of reoperation. Controversy remains over who is at highest risk of intra-abdominal sepsis and may thereby benefit from fecal diversion at the time of ileocecal resection. The aims of this study were to determine 1) risk factors for intra-abdominal sepsis following ileocolic resection and 2) if risk factors are consistent across inflammatory bowel disease (IBD) referral centers.
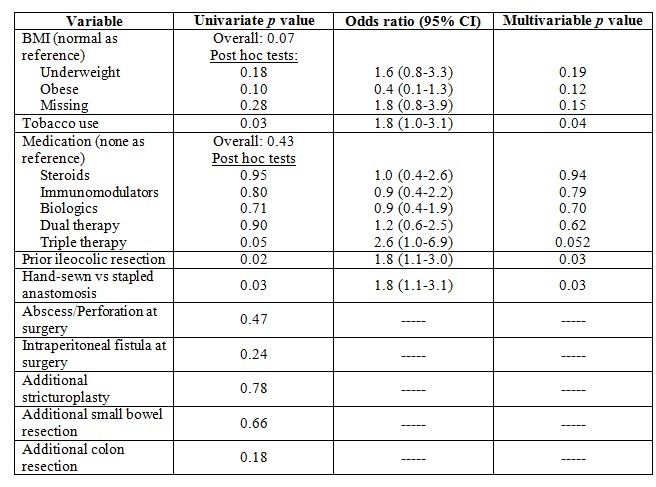
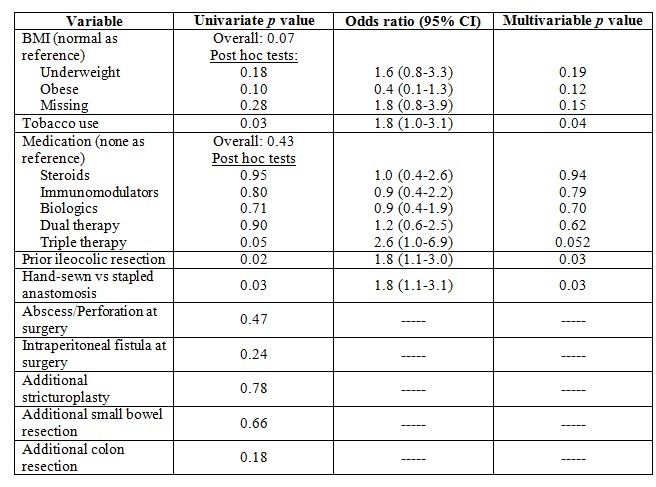
Methods: A retrospective chart review was conducted of all adult patients undergoing ileocolic resection with primary anastomosis for CD between January 2010 and August 2017 at three international IBD referral centers. Patients diverted at the time of ileocolic resection were excluded. Intra-abdominal sepsis was defined as an intraperitoneal abscesses or anastomotic leak. Dual immunosuppression was considered any combination of the following: corticosteroids (at operation), immunomodulatory agents or biologic (within 12 weeks of surgery); triple immunosuppression was the use of all three. Univariate and multivariable analysis was conducted to determine risk factors for intra-abdominal sepsis.
Results: 834 patients (53% female) with a median age of 39 years (range, 18-86) underwent ileocolic resection for CD. The overall rate of intra-abdominal sepsis was 8% (site 1: 6%, site 2: 9%, and site 3: 10%). On univariate analysis, tobacco use, prior ileocolic resection, and a hand-sewn anastomosis were associated with intra-abdominal sepsis. On multivariable analysis, all three were independent risk factors for intra-abdominal sepsis (Table). The rate of intra-abdominal sepsis was 4%, 9%, 12%, and 20% for 0, 1, 2, and 3 risk factors respectively (p<0.01 for 1, 2 and 3 risk factors versus 0 risk factors).
Risk factors associated with intra-abdominal sepsis differed between the three sites. Being underweight (BMI<18.5) was associated with intra-abdominal sepsis at site 1 (p<0.01), while prior intestinal resection (adjusted odds ratio 2.3; 95% confidence interval, 1.2-4.5) was independently predictive of intra-abdominal sepsis at site 2, and no risk factors were associated with intra-abdominal sepsis at site 3.
Conclusion: Tobacco use, prior intestinal resection and a hand-sewn anastomosis are independently associated with intra-abdominal sepsis following ileocolic resection in CD. Smoking cessation preoperatively should be emphasized and patients with multiple risk factors may benefit from fecal diversion. Interestingly, risk factors varied across three large IBD referral centers.
Back to 2018 Program and Abstracts
|