|
Back to 2018 Program and Abstracts
EFFECT OF PERIOPERATIVE HIGH CONCENTRATION OXYGEN SUPPLEMENTATION ON POSTOPERATIVE SURGICAL SITE INFECTION IN PATIENTS UNDERGOING ELECTIVE COLORECTAL SURGERY- A RANDOMIZED CONTROLLED TRIAL
Vikram Kate*1, Mayank Mangal1, Subair Mohsina1, Sathasivam Sureshkumar1, Pankaj Kundra2
1Department of Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, Pondicherry, India; 2Department of Anesthesiology and Critical Care, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India
Introduction: This study was carried out to investigate the effect of perioperative high oxygen concentration (80% FiO2) on Surgical Site Infection (SSI) in patients undergoing elective colorectal surgery.
Methods: This was a single centre, prospective, parallel arm, double blind; superiority randomized controlled trial carried out over a period of two years. All patients of age >18 years, undergoing elective colorectal surgery under general anaesthesia were included. Patients undergoing minor colorectal procedures, patients with evidence of infection, malnutrition, respiratory illness and those who are unfit for general anaesthesia were excluded. Stratified block randomization was done and allocation was carried out in 1:1 ratio into 80% FiO2 and 30 % FiO2 group. Stratification was done based on preoperative plan of stoma vs. no stoma. Patients in the 80 % FiO2 group received high concentration oxygen (80% oxygen + 20% nitrogen) intraoperatively via endotracheal tube and postoperatively up to 6 hours through non-rebreathing mask. Patients in the 30% FiO2 group received standard concentration (30% oxygen + 70% nitrogen) intraoperatively and supplement oxygen postoperatively through standard face mask. The patients were assessed daily for development of SSI using the ASEPSIS criteria. Primary outcome measure was incidence of SSI and secondary outcome measures were the day of the detection of SSI, Grade of SSI, incidence of anastomotic leak, postoperative day of return of bowel functions, postoperative day of ambulation and length of hospitalization.
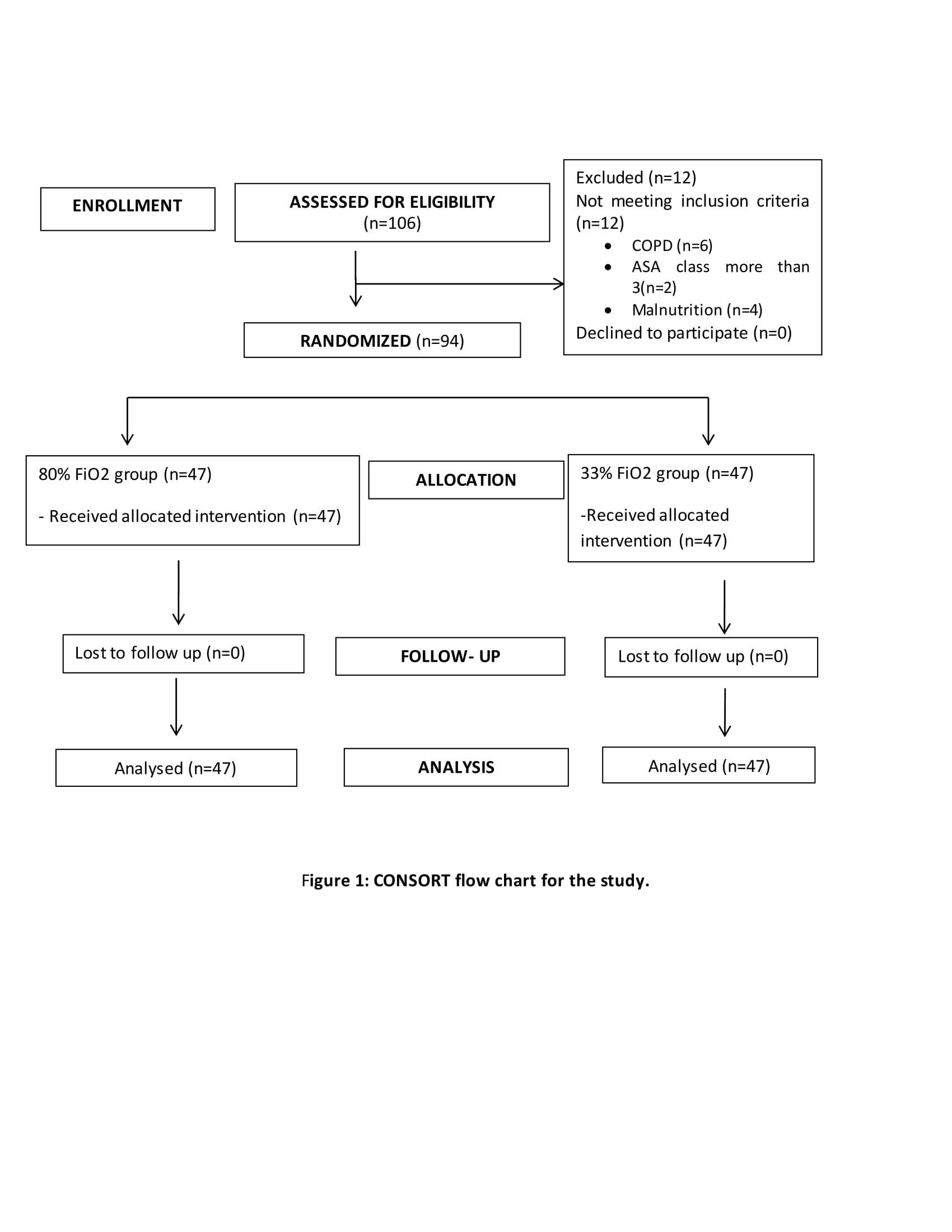
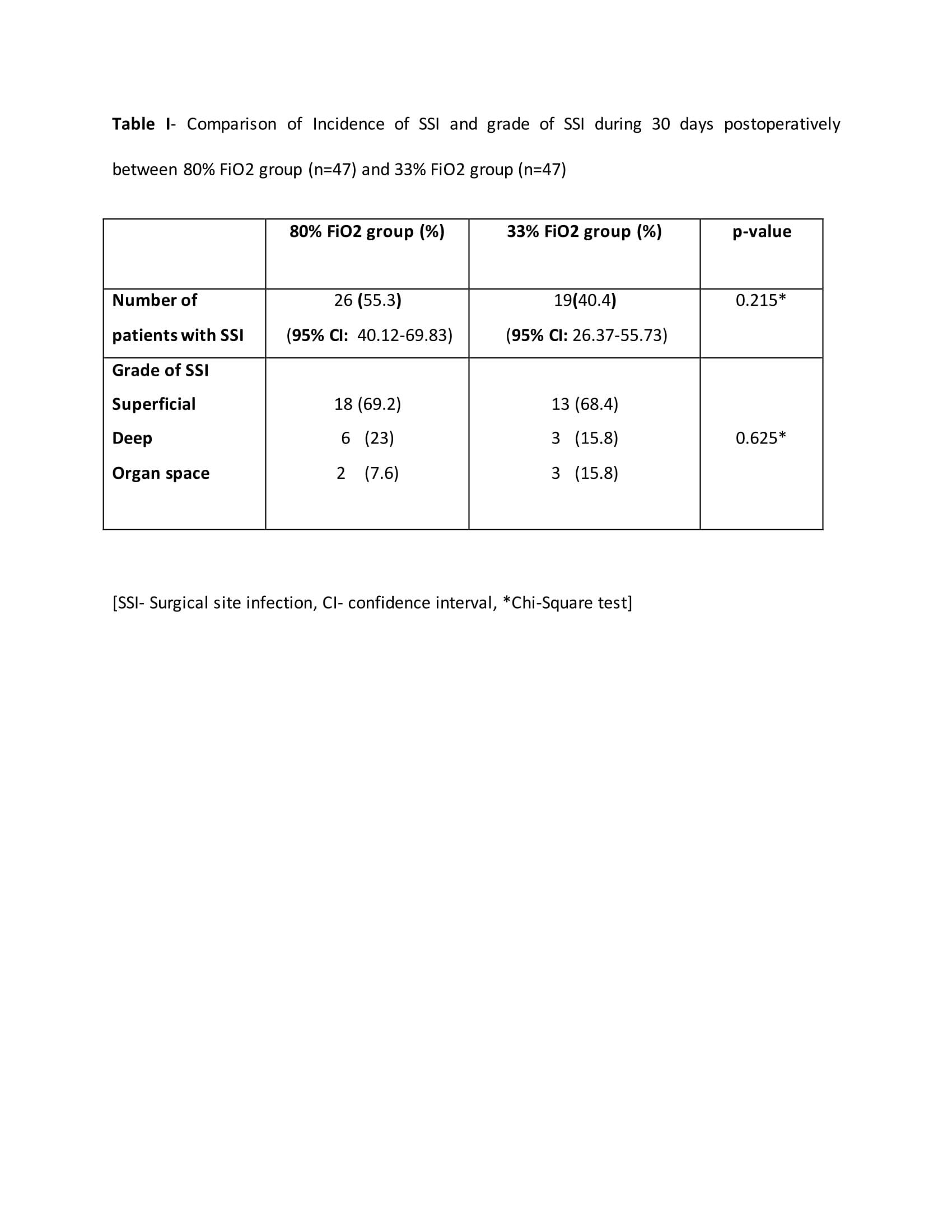
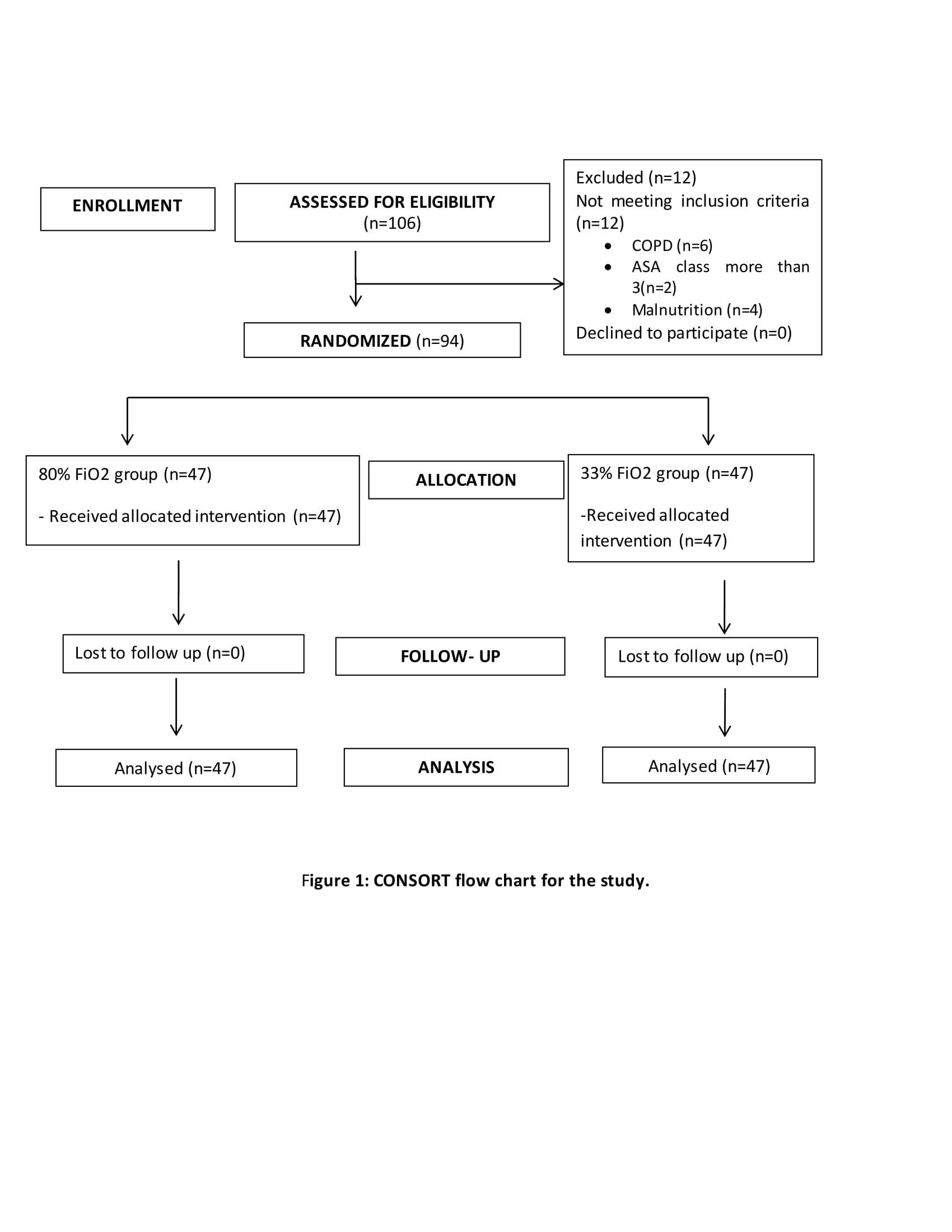
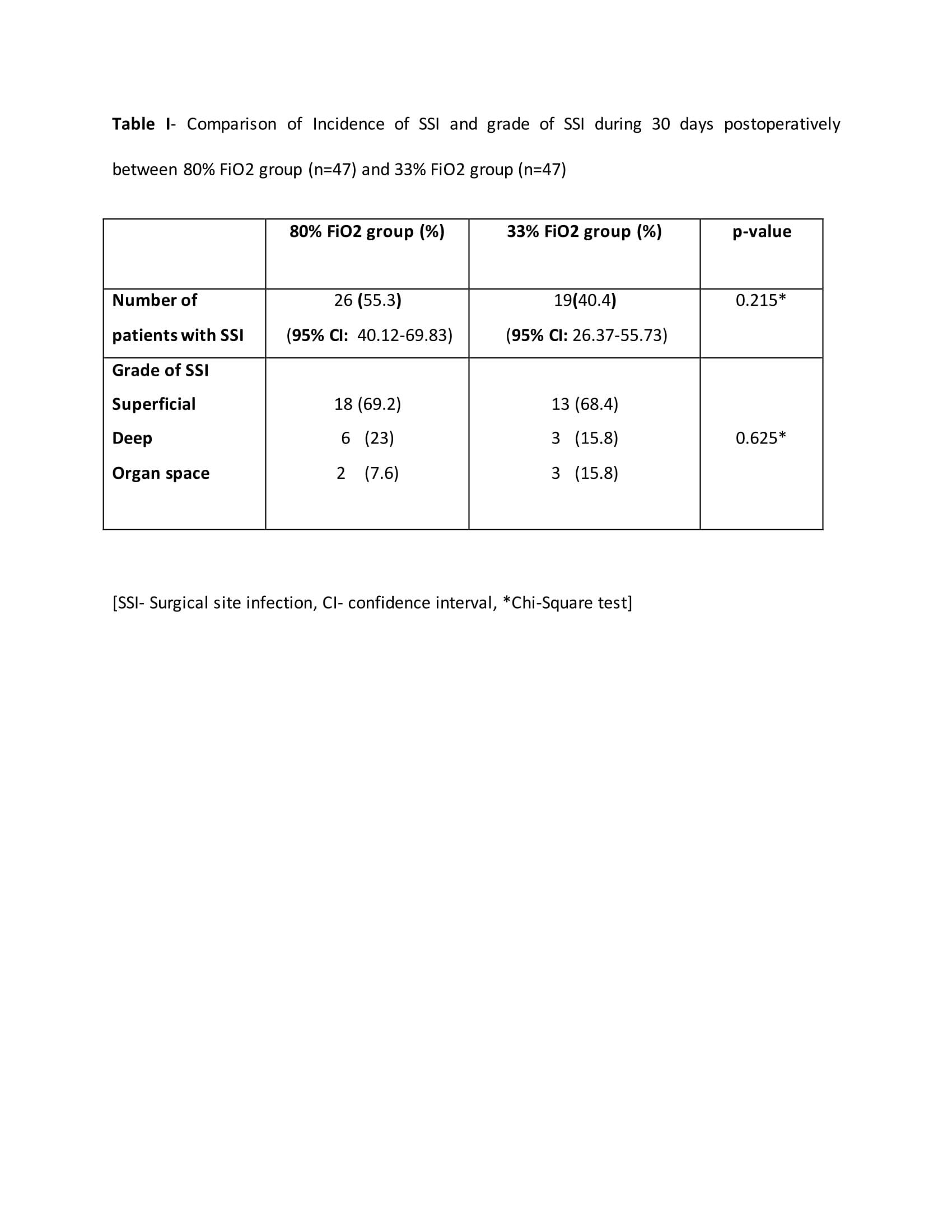
Results: A total of 94 patients were included in the study, 47 patients each in group (Figure1). The two groups were comparable in the demographic and clinicopathological characteristics such as age, gender, ASA grade, primary diagnosis, duration of surgery and type of anastomosis. The overall incidence of SSI was 47.87%. The SSI rates were similar between the 80% FiO2 and 30 % FiO2 groups (55.32% vs. 40.43%; p=0.148). The grades of SSI between the two groups were comparable (superficial: 68% vs. 68.4%; deep: 28% vs. 16%; organ space: 4 % vs. 15%; p=0.30) (Table1). The anastomotic leak rate was similar between the two groups (1/47 vs. 2/47; p=0.27). The mean day of detection of SSI (2.96 + 3.451 vs. 2.51�+ 3.928; p=0.246), postoperative day of return of bowel functions (2.20�+ 0.542 vs. 2.13�+ 0.582; p=0.54), postoperative day of ambulation (4.15�+ 0.868 vs. 4.18�+ 1.284; p=0.97) and length of hospitalization (16.09�+ 8.174 vs. 16.72�+ 10.336; p=0.862) was similar between the two groups.
Conclusion: The perioperative high oxygen concentration therapy does not reduce surgical site infection in patients undergoing elective colorectal surgery.
Back to 2018 Program and Abstracts
|