|
Back to 2018 Program and Abstracts TRANSORAL OUTLET REDUCTION FOR THE MANAGEMENT OF WEIGHT REGAIN AND DUMPING SYNDROME AFTER ROUX-EN-Y GASTRIC BYPASS. Lea Fayad*1, Roberto Oleas1, Sindhu Barola1, Christine Hill2, Dilhana S. Badurdeen1, Margo K. Dunlap1, Michael Schweitzer1, Anthony N. Kalloo1, Mouen A. Khashab1, Vivek Kumbhari1 1Johns Hopkins Hospital, Baltimore, MD; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD
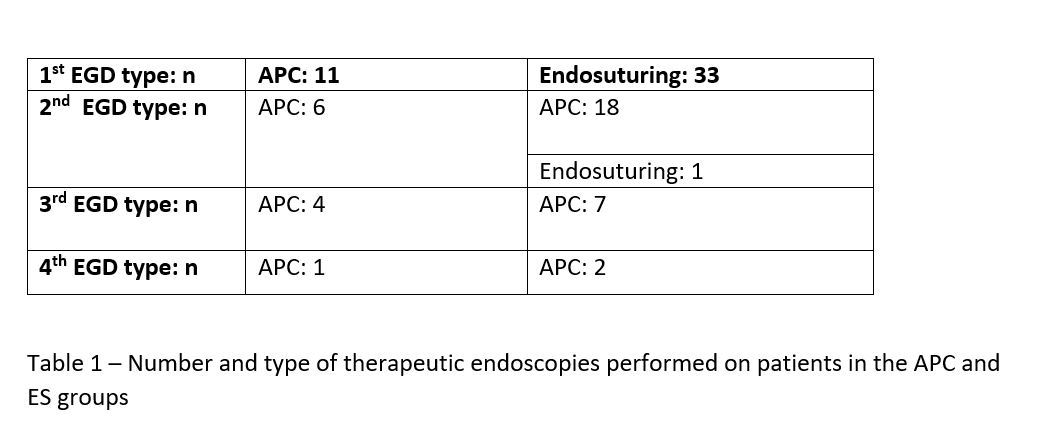
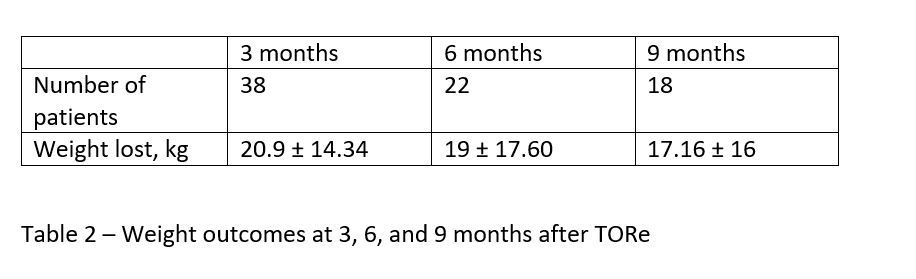
Background: Weight regain and dumping syndrome (DS) are long term complications of Roux-en-Y Gastric Bypass (RYGB), which are associated with a dilated gastrojejunal (GJ) anastomosis. Transoral outlet reduction (TORe) is an endoscopic procedure that reduces the GJ outlet size by using devitalization with argon plamsa coagulation and/or endoscopic suturing (ES). It has proven to be a safe and effective procedure in the management of weight regain with dilated GJ post-RYGB. Aims: To evaluate the efficacy and safety of TORe for the management of weight regain and DS post-RYGB. Methods: A retrospective review of a prospectively maintained database was performed. Consecutive patients who underwent TORe for weight regain or DS post-RYGB with a dilated GJ between September 2015 and September 2017 at a single academic center were reviewed. ES was performed using a novel two-fold running suture technique. The patients underwent no diet or lifestyle intervention and no medical management for their weight regain. The GJ was measured. If dilated, patients applied to insurance for TORe using ES with argon plasma coagulation (APC). If accepted, ES was performed. If denied, patients underwent APC only. All patients then had a follow up EGD. If outlet remained dilated, APC was performed and patients had another follow-up EGD scheduled. Patient symptoms were assessed using the Dumping Symptom Rating Scale (DSRS) before and after TORe. Patient weights were followed at 3, 6, and 9 months. Results: In total, 44 patients (40 female) underwent TORe (age: 48.6 ± 9 years). Patients on average presented for TORe 6.34 ± 4.65 years after RYGB. BMI at baseline was 40.6 ± 9.92 kg/m2. Indications for TORe included DS (7%), weight regain (44.2%), or both (48.8%). Weight regained was 57.93 ± 34.77 lbs from their nadir after RYGB. Patients had regained 43.68 % ± 21.1 of their lost weight after their nadir after RYGB. 33/44 patients underwent ES as their first procedure. Overall, out of 44 patients, 29 patients required a 2nd endoscopy, 13 required a 3rd endoscopy, and 3 required a 4th endoscopy (Table 1). 4 patients required balloon dilation on the second endoscopy due to gastric stenosis and 2 required balloon dilation on the third endoscopy as well. Size of the outlet at first EGD was 27.3 (25.2-29.3) mm and was significantly smaller 13.6 (11.7-15.5) mm at second EGD (p < .000). Weight outcomes at 3, 6, and 9 months can be seen in table 2. DSRS scores were significantly reduced from a median of 31 (11-85) before the procedure to 21 (11-49) after the procedure (p <0.000). Conclusion: TORe is an effective technique for the management of weight regain and/or DS in patients with a dilated GJ after RYGB. Mutiple endoscopic sessions may be required for optimal outlet reduction. Back to 2018 Program and Abstracts |
|||||||||||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.