|
 |
Back to 2018 Program and Abstracts
OUTCOMES OF RADIATION INDUCED SQUAMOUS CELL CARCINOMA ARE SUGGESTIVE OF A VERY AGGRESSIVE DISEASE
Tamar B. Nobel*1, Arianna Barbetta1, Francisco Schlottmann2, Manjit S. Bains1, Matthew Bott1, James Isbell1, Smita Sihag1, Marco G. Patti2, David R. Jones1, Daniela Molena1
1Department of Surgery, Thoracic Surgery Service, Memorial Sloan Kettering Cancer Center, New York, NY; 2Department of Surgery, Division of GI Surgery, University of North Carolina, Chapel Hill, NC
Objective:
Radiation induced esophageal squamous cell cancer (ESCC-R) is a rarely encountered disease; however, incidence is expected to rise as a result of increasing indications for use of chest radiation. Treatment is limited by toxicity associated with reirradiation and the complexity of surgical dissection in a previously radiated field. Although optimal treatment strategies are lacking, prognosis is considered comparable to primary esophageal squamous cell carcinoma (ESCC). The purpose of this study was to characterize a cohort of patients with ESCC-R, and compare their perioperative and long-term survival to patients with primary ESCC.
Methods:
A retrospective review was performed of all patients with esophageal squamous cell carcinoma at a single institution between 1995 and 2017 to identify patients with a previous history of radiation therapy (> 5 years delay). Clinicopathologic characteristics, treatment and outcomes of patients with ESCC-R were compared to those of patients with primary ESCC. Continuous variables were compared using the Mann-Whitney U test and categorical variables using the Fisher's exact test. Overall and disease free survival (OS and DFS, respectively) were evaluated using the Kaplan-Meier method.
Results:
We identified 50 patients with ESCC-R (67% female, median age 68 years, IQR 59.8-75). Patients received a median radiation dose of 6060 cGY (4680-6965) with indications being head and neck (34%), breast (32%) or thoracic cancer (10%); and lymphoma (24%). Median time from radiation to ESCC-R diagnosis was 17.8 years (9-27.9). Most of the patients were stage II/III at diagnosis (94%). Treatment included surgery +/- adjuvant chemotherapy (34%), definitive chemoradiation (24%), neoadjuvant chemotherapy (14%) or chemoradiation (nCRT) (18%) followed by surgery, and chemotherapy or radiation therapy alone (10%).
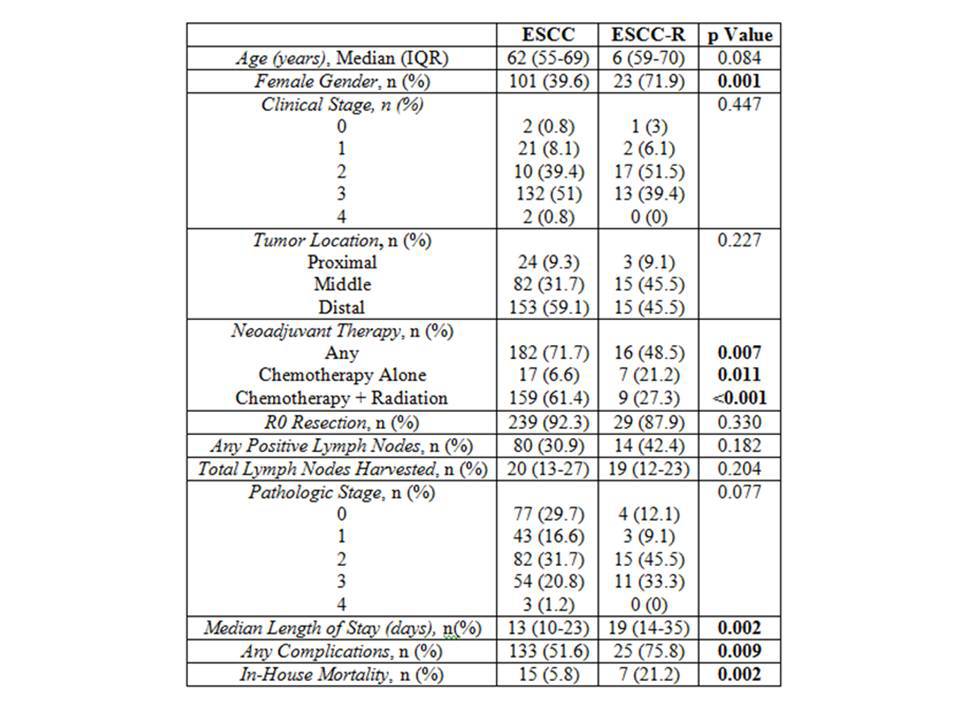
Comparison between patients with ESCC-R and ESCC who underwent surgery is listed on Table 1. ESCC-R patients were less likely to receive neoadjuvant therapy (48.5 vs 71.4%, p=0.008), and specifically, nCRT (27.3 vs 61.4%; p<0.001). ESCC-R patients had more postoperative complications and higher incidence of in-hospital mortality (75.8 vs 51.4%, p=0.008; and 21.2 vs 5.9%, p=0.002, respectively). Most ESCC-R patients who died postoperatively received neoadjuvant radiation (4/7, 57%).
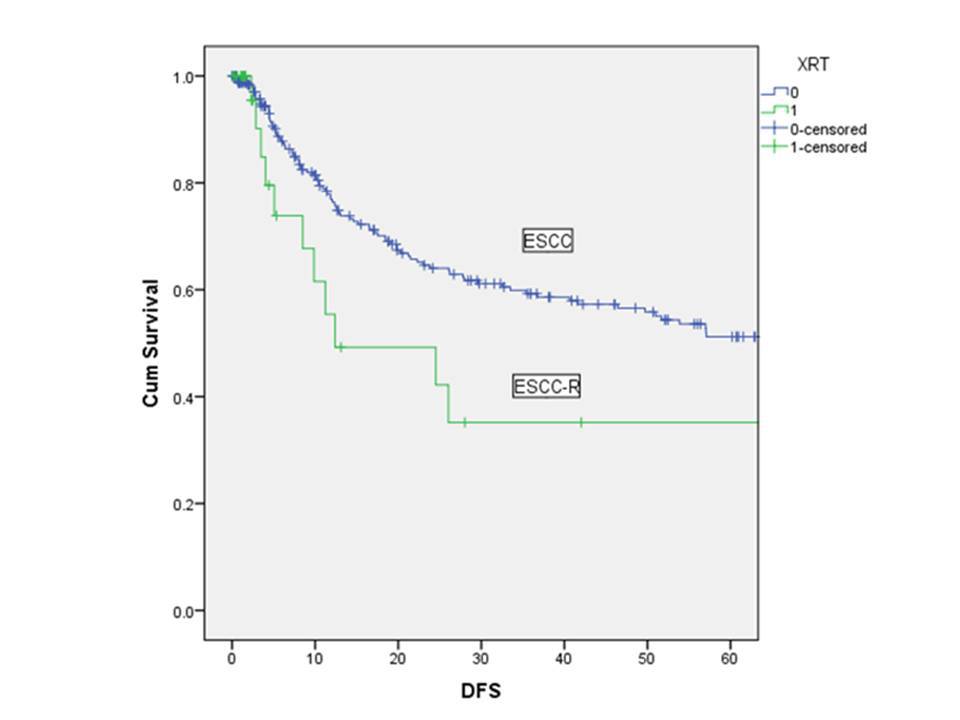
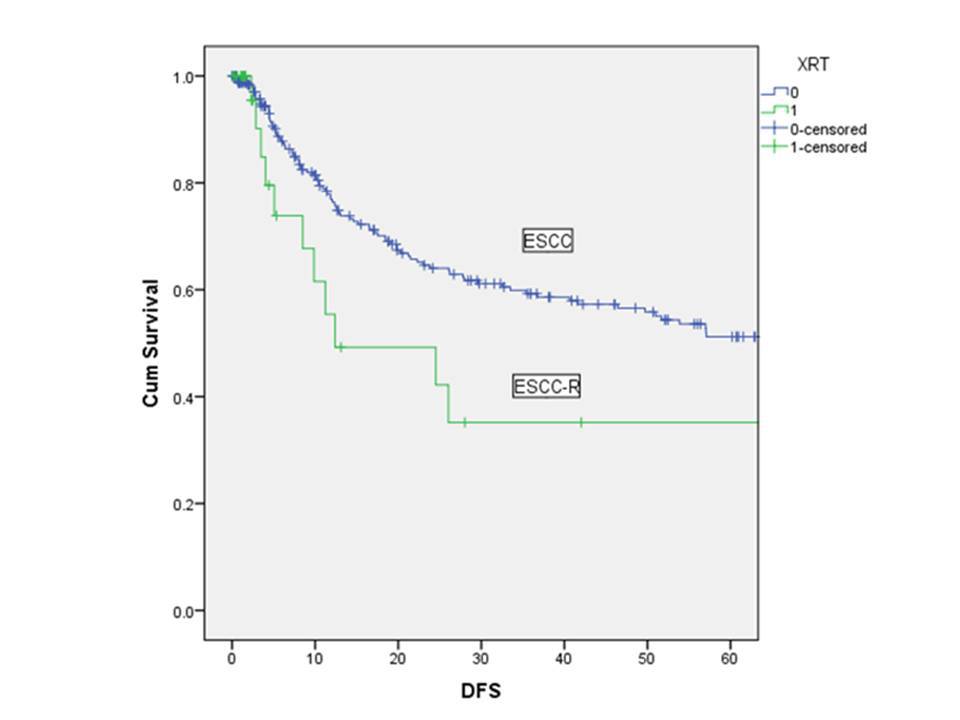
Median DFS and OS was lower for patients with ESCC-R (12.4 vs 101.3 months; p=0.046 and 9.8 vs 43.2; p<0.001, respectively) (Figure 1). Amongst ESCC-R patients, no difference in survival was observed between patients who did and did not receive neoadjuvant treatment.
Conclusion:
ESCC-R is associated with significant postoperative morbidity and mortality, and worse long-term survival than ESCC. Although the role of undertreatment must be further evaluated, our results suggest that ESCC-R may be a more aggressive disease.
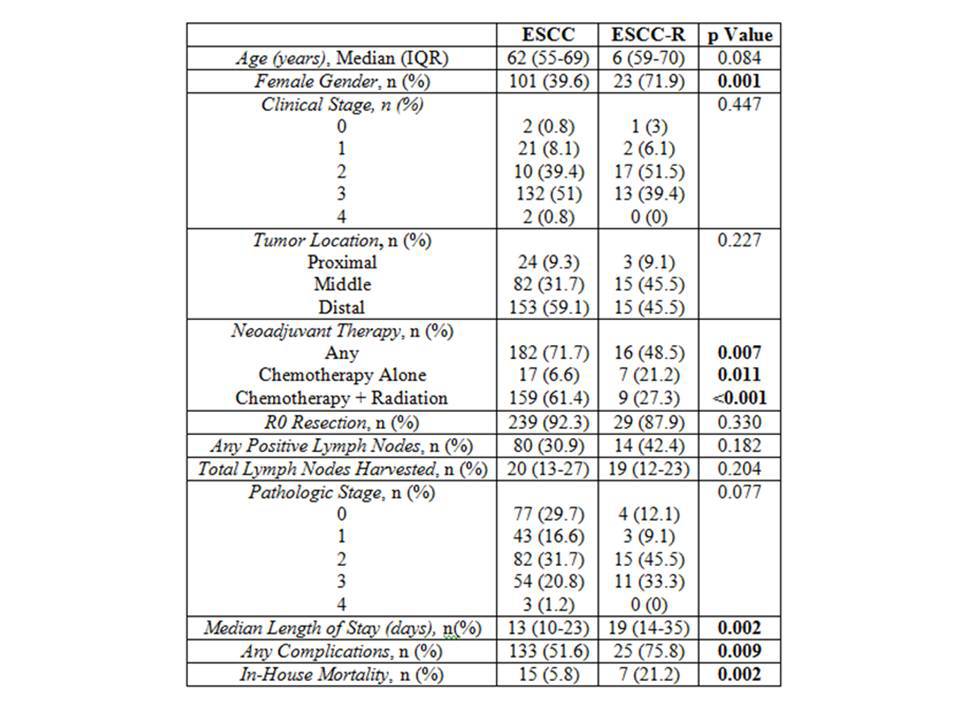
Table 1. Clinicopathologic Comparison of ESCC-R and ESCC
Back to 2018 Program and Abstracts
|