|
 |
Back to 2018 Program and Abstracts
INFLUENCE OF RADIATION DOSE ON UNDERGOING ESOPHAGECTOMY FOR LOCALLY ADVANCED ESOPHAGEAL CANCER
Mickey S. Ising*1,2, Jaimin Trivedi2, Katy Marino2, Adam Rojan4, Neal Dunlap3, Victor van Berkel2, Matthew Fox2
1Department of Surgery, University of Louisville, Louisville, KY; 2Department of Cardiovascular and Thoracic surgery, University of Louisville, Louisville, KY; 3Department of Radiation Oncology, University of Louisville, Louisville, KY; 4Division of Medical Oncology and Hematology, Department of Medicine, University of Louisville, Louisville, KY
Neoadjuvant chemoradiotherapy followed by resection is standard of care for patients with locally advanced esophageal cancer, however, a significant portion of these patients do not undergo surgical intervention. We sought to identify factors associated with failure to undergo esophageal resection in patients with locally advanced esophageal cancer receiving chemoradiotherapy.
The National Cancer Database was queried for patients diagnosed between 2010-2015 with squamous cell or adenocarcinoma esophageal cancer, located in the middle or lower esophagus, and stage T1N1M0 or T2-3N0-1M0 who were treated with chemoradiotherapy. Patients were excluded if surgical intervention was not part of the planned first course treatment or was limited to local tumor destruction. Patients were stratified into low dose (41.4 Gy) or high dose radiation (50.0 or 50.4 Gy) groups. Logistic analysis identified predictors of patients failing to undergo esophagectomy. Cox-regression analysis assessed impact on survival from diagnosis.
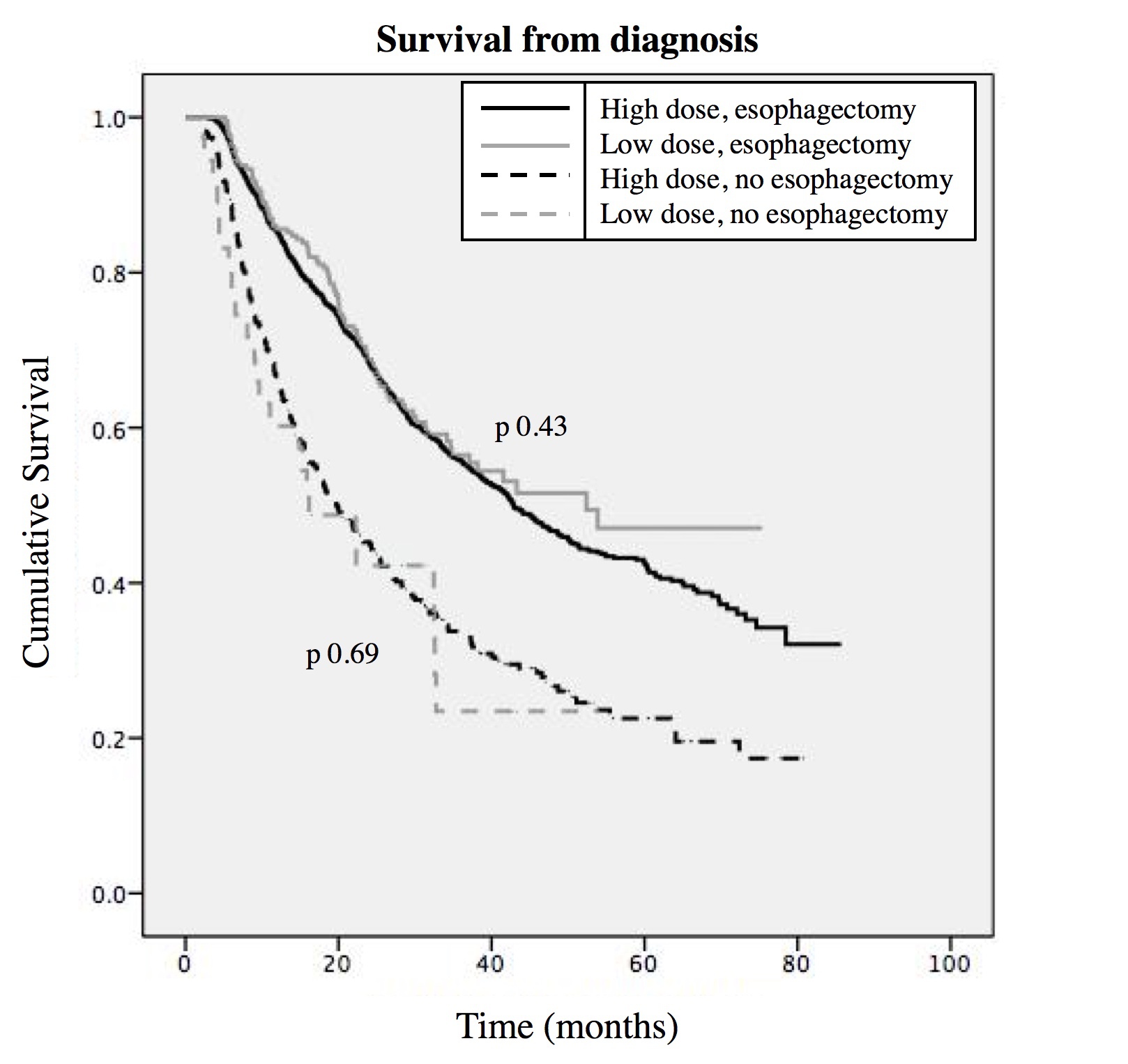
A total of 2,996 patients met inclusion criteria for the study, with 2,474 (83%) undergoing esophagectomy. Of the 522 patient that did not receive surgery, it was contraindicated due patient risk factors in 260 (51%). Factors associated with failure to undergo resection included: high dose radiation, squamous cell histology, greater Charlson Comorbidity score, older age, living closer to the treatment facility, having medicaid or no insurance compared to private, and not being at an academic/research or integrated cancer network (ICN) program (Table 1). There was no difference in the portion of patients who had complete pathologic response between low (5.5%) and high dose radiation (4.7%, p 0.47). Undergoing esophagectomy led to increased survival, however, when stratified by resection or not, there was no difference between radiation doses (Figure 1). Cox regression analysis showed improved survival in those who underwent esophagectomy, were younger, and were treated at an academic/research or ICN program. Patients who received low dose radiation had surgery earlier (129.6±32.9 vs 143.4±37.7 days, p<0.001), but had no difference in postoperative stay (12.4±10.6 vs 12.5±11.3 days, p 0.749), unplanned 30-day readmission (6.3 vs 4.4%, p 0.103), or mortality at 30 days (2.5 vs 3.5%, p 0.559) or 90 days (5.0 vs 7.7%, p 0.148), as compared to high dose.
It is well established that patients with locally advanced esophageal cancer have improved survival with surgical resection. This study shows that higher radiation dosage is associated with failing to undergo esophagectomy while providing no survival benefit for both patients who underwent surgery and those who did not. Ultimately, using reduced radiation dosages as part of neoadjuvant chemoradiotherapy for locally advanced esophageal cancer, may lead to increased resection and subsequent survival.
Table 1: Predictors of failure to undergo esophagectomy
| | Hazard Ratio | 95% Conf limits | p Value | | African American | 1.296 | 0.796-2.111 | 0.298 | | >21% no high school degree | 1.224 | 0.866-1.730 | 0.253 | | Lowest income quartile | 0.905 | 0.641-1.278 | 0.571 | | Academic/research/ICN program | 0.537 | 0.436-0.660 | <0.001 | | Age | 1.088 | 1.072-1.105 | <0.001 | | Distance from hospital | 0.997 | 0.994-0.999 | 0.003 | | Charlson Combordity score | 1.330 | 1.158-1.527 | <0.001 | | Squamous cell histology | 1.878 | 1.389-2.539 | <0.001 | | Male | 1.189 | 0.897-1.576 | 0.228 | | Middle esophageal cancer | 1.420 | 1.045-1.929 | 0.025 | | High radiation dose (50 or 50.4Gy) | 1.663 | 1.192-2.320 | 0.003 | | Insurance type | | | | | Private | REF | REF | REF | | Medicare | 1.054 | 0.797-1.393 | 0.711 | | Medicaid | 2.419 | 1.555-3.763 | <0.001 | | None | 2.13 | 1.057-4.291 | 0.034 | | Other | 2.423 | 1.428-4.113 | 0.001 |
ICN - Integrated Cancer Network 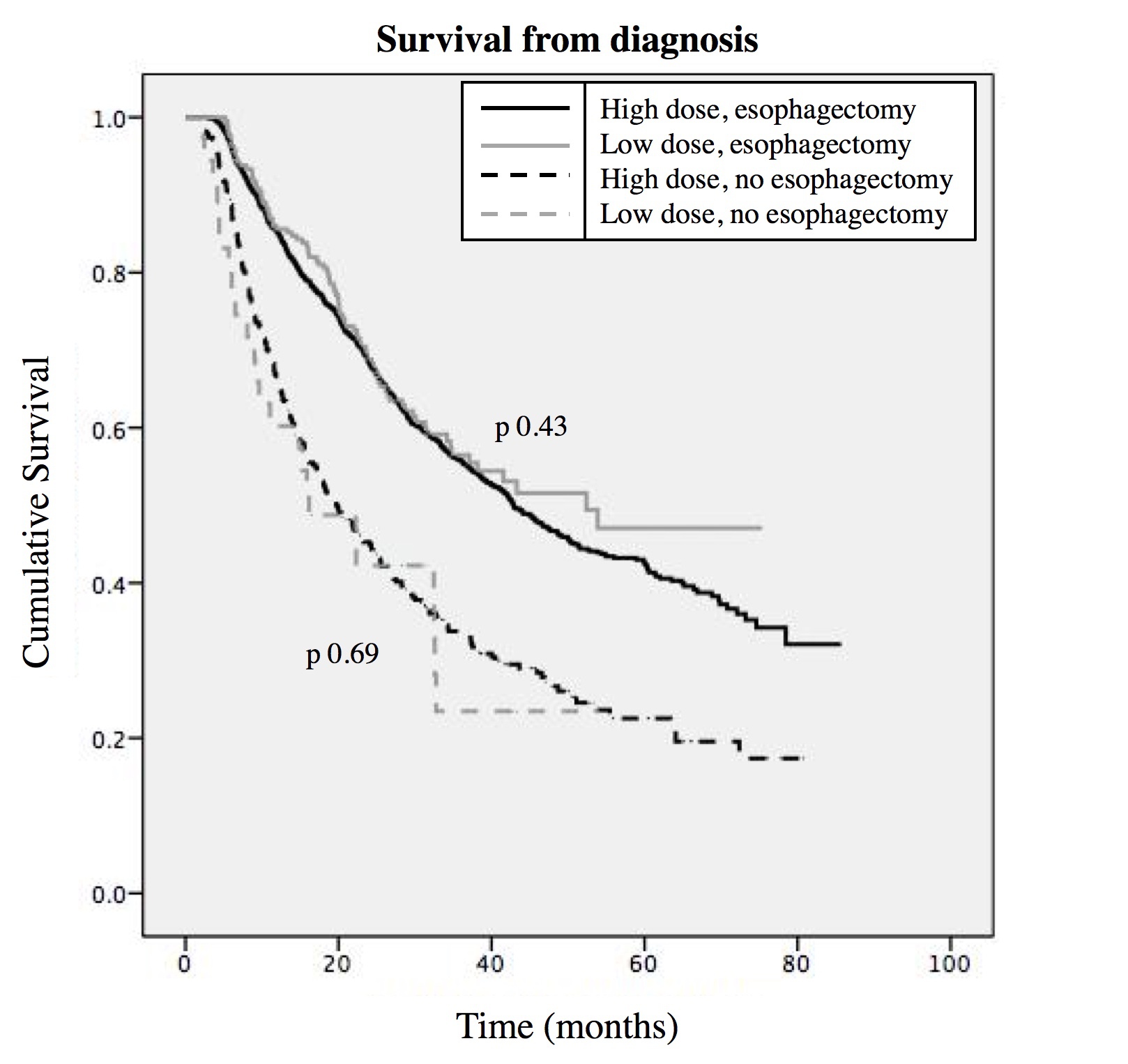 Figure 1: Cumulative survival for patients undergoing or not undergoing esophagectomy with high dose (50 or 50.4Gy) or low dose (41.4Gy) radiation.
Back to 2018 Program and Abstracts
|