|
Back to 2018 Program and Abstracts
OUTCOMES AFTER PALLIATIVE STENTING VERSUS STOMA CREATION FOR MALIGNANT BOWEL OBSTRUCTION
Patrick T. Dolan*1, Matthew Symer1, Heather L. Yeo1,2
1Surgery, New York-Presbyterian/Weill-Cornell Medical Center, New York, NY; 2Healthcare Policy and Research, Weill Cornell Medicine, New York, NY
Introduction: Palliation of malignant large bowel obstruction can be accomplished with either colonic stenting or stoma creation, but the optimal approach to this problem is not yet defined. We compared the outcomes of patients undergoing colonic stenting and stoma creation for emergent malignant large bowel obstruction.
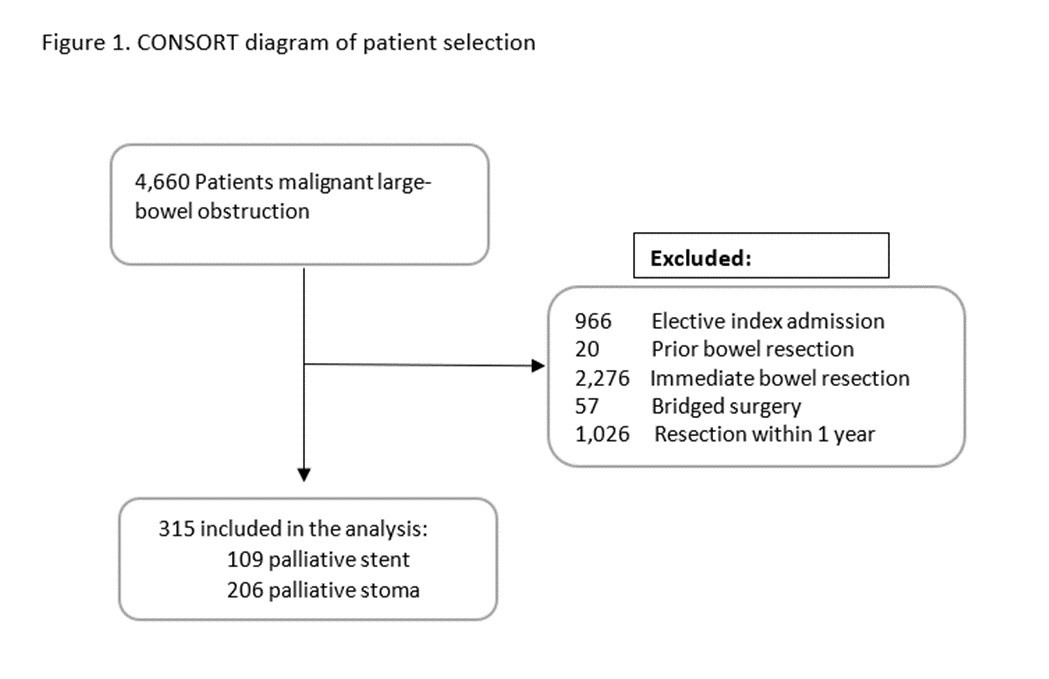
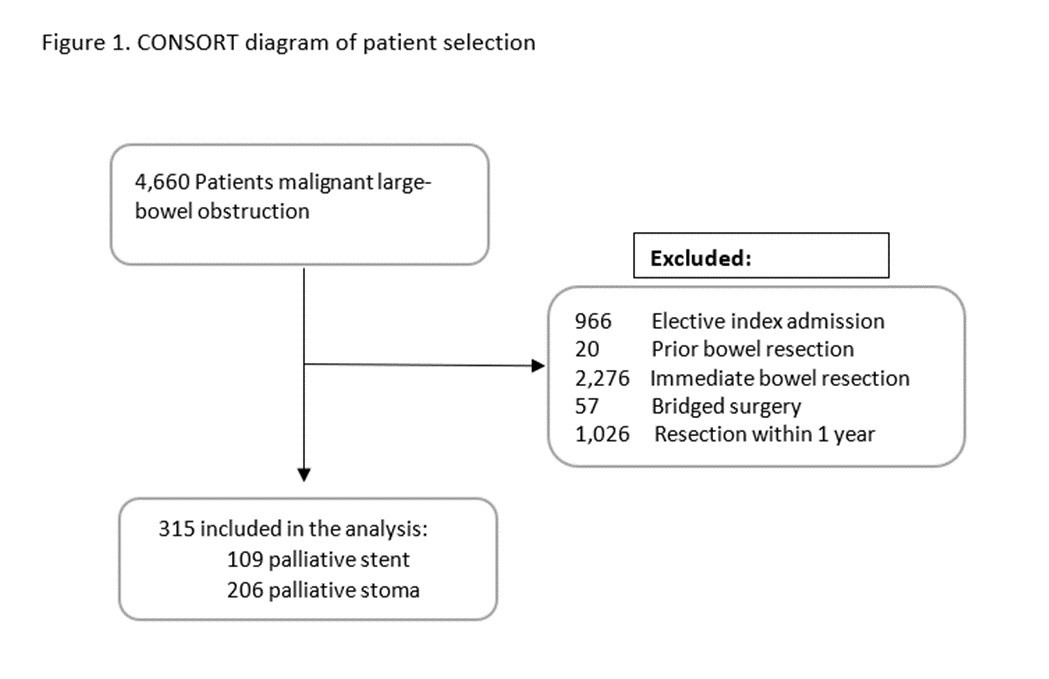
Methods: We performed a secondary data analysis of the Medicare-Linked Surveillance Epidemiology and End Results (SEER) database. Patients were included if they had an emergent hospitalization for large bowel obstruction secondary to colorectal cancer between October 2009 and December 2014, and subsequently had either a stent or stoma creation only. To ensure these were palliative procedures, patients who had elective resection within one year were excluded. Data were analyzed using a multivariable logistic regression. Primary outcome was overall survival at 90 days. Secondary outcomes included 90-day disease specific survival, in-hospital mortality, complications, length of stay, discharge disposition, and readmission within 90 days.
Results: 315 patients were identified, 109 of whom were stented and 206 received a stoma. Average age was similar in the two groups (stoma group 79.3 years vs stent 79.6 years, p=0.81), as was gender (stoma 46.1% male vs stent 51.4%, p=0.37), and race (stoma 77.7% non-Hispanic white vs stent 78.9%, p=0.68). A higher proportion of patients in the stent group had stage 4 tumors (stoma 40.3% vs stent 65.1%, p<0.001). Median overall survival was 4 months, and was not different between groups (with stoma as reference, stenting adjusted HR 0.98 95%CI 0.75-1.30, p=0.91). Similarly, cancer-specific survival was 3 months and not different (stenting adjusted HR 1.34 95%CI 0.67-2.66), p=0.40). In multivariable regression, patients undergoing palliative stenting were less likely to have a prolonged length of stay (OR 0.24 95%CI 0.11-0.57, p<0.05) or be discharged somewhere other than home (OR 0.02 95%CI 0.00-0.08, p<0.05). There were no differences in procedural complications (OR 0.18 95%CI 0.03-1.10), in-hospital mortality (OR 0.34 95%CI 0.08-1.43), or readmission within 90 days (OR 0.86 95%CI 0.47-1.59).
Conclusion: In patients with colorectal cancer and large bowel obstruction, palliative stenting and stoma creation are associated with similar overall and cancer-specific survival at 90 days. Stenting was superior to stoma in terms of discharge home and length of stay, without any difference in procedural complications, in-hospital mortality, or readmission within 90 days.
Back to 2018 Program and Abstracts
|