|
 |
Back to 2018 Program and Abstracts
APPLICATION OF THE AAST EGS GRADE FOR SMALL BOWEL OBSTRUCTION TO A MULTI-NATIONAL PATIENT POPULATION
Matthew C. Hernandez*1, Arianna Birindelli2,5, Nadeem Haddad1, John L. Bruce3, Johannes Buitendag3, Wanda Bekker3, Abraham Ras3, Victor Kong3, Mircea Beuran4, Johnathon Aho1, Ionut Negoi4, Damian Clarke3, Salomone Di Saverio5,6, Martin D. Zielinski1
1Surgery, Mayo Clinic, ROCHESTER, MN; 2Queen Elizabeth University, Birmingham, United Kingdom; 3Pietermaritzburg Metropolitan Complex, Pietermaritzburg, South Africa; 4Carol Davila University of Medicine and Pharmacy of Bucharest, Bucharest, Romania; 5Maggiore Hospital, Bologna, Italy; 6Addenbrookes Hospital, Cambridge, United Kingdom
Introduction:
The American Association for the Surgery of Trauma (AAST) grading system for adhesive small bowel obstruction (ASBO) demonstrated validity within the USA. We assessed the ability of the AAST grade to estimate ASBO severity in a diverse global population and correlate with key clinical outcomes.
Methods:
Multi-center retrospective review (2012-2016) was performed at four centers: Minnesota USA, Bologna Italy, Pietermaritzburg South Africa, and Bucharest Romania. Adult patients (age≥18) with ASBO were identified. Baseline demographics, physiologic parameters (heart rate, blood pressure, and respiratory rate), laboratory results (lactate, hemoglobin, creatinine, and leukocytosis), operative and imaging details, length of stay, and Clavien-Dindo complications were collected. Grades were assigned by independent reviewers at each participating center using imaging and operative findings. Univariate and multivariable analyses with odds ratio (OR) and 95% confidence intervals (CIs) were performed.
Results:
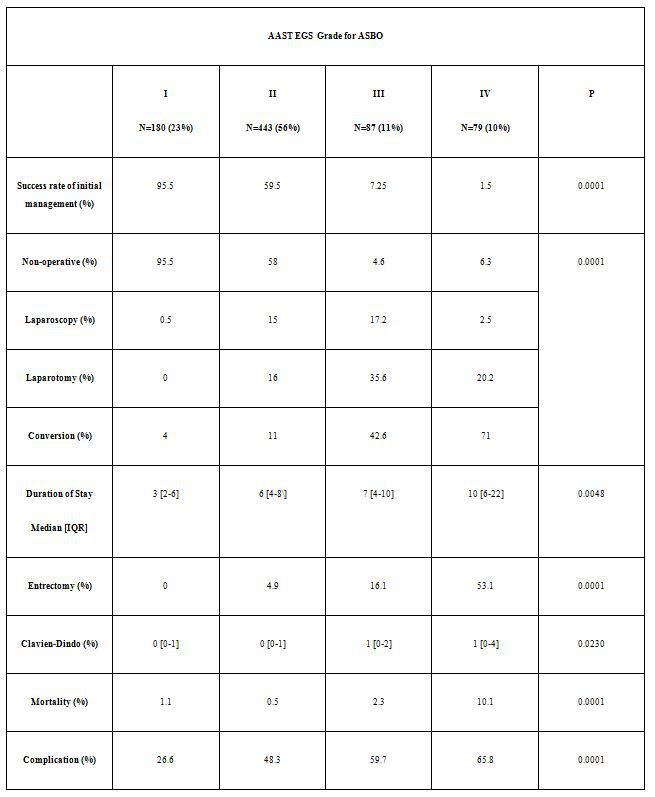
A total of 789 patients were identified. Median age was 58 [40-75] years, 48% were female, and mean BMI was 26.4±7.1. Grades included I (n=180, 23%), II (n=443, 56%), III (n=87, 11%), IV (n=79, 10%). Initial management included: Gastrografin challenge (n=287, 36%), nasogastric suction alone (n=332; 42%), laparotomy (n=104, 13%), and laparoscopy (n=66, 9%). Non-operative management success rate was 58%. Resoultion of ASBO via initial management diminished for increasingly severe disease, Table. For laparoscopic management, the conversion to laparotomy rate was 4.3%. Overall mortality and complication rates were 2% and 46% respectively. Overall median [IQR] duration of stay was 6 [4-8] days. There was a 5% temporary abdominal closure rate. Disease severity was most acute in South Africa, with 27% of patients demonstrating grade IV disease compared to Italy (2%), USA (9.6%) and Romania (3.3%). The associations of increasing AAST EGS grade for ASBO is presented in Table. On regression, factors independently associated with increased risk for mortality (all p<0.05) included disease severity (relative to grade I): grade III (OR 4.4 95%CI 1.1-7.3), grade IV (OR 7.4 95%CI 1.7-9.4), post-operative pneumonia (OR 5.6 95%CI 1.4-11.3) and failing non-operative management (OR 2.4 95%CI 1.3-6.7)
Conclusion:
Retrospective cohort comparison can be performed using the AAST EGS grade.The AAST ASBO grade describes disease severity in a multi-national population. Increasing disease severity was associated with several clinical outcomes including mortality and complications. Extension of the AAST EGS grade to broader populations is possible. Incorporating the AAST EGS grade will continue to provide improved disease severity classification for prospective analyses of operative and guideline based non-operative management.
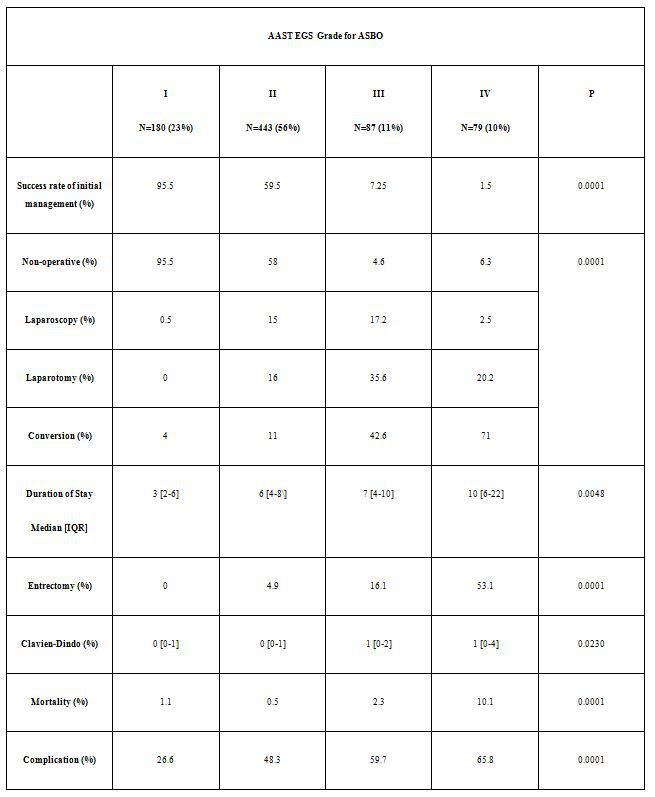
Table
Back to 2018 Program and Abstracts
|