|
Back to 2018 Program and Abstracts
SURGICAL RESECTION FOR RECURRENCE AFTER TWO-STAGE HEPATECTOMY FOR COLORECTAL LIVER METASTASES IS ASSOCIATED WITH IMPROVED SURVIVAL
Heather A. Lillemoe*, Yoshikuni Kawaguchi, Georgios Karagkounis, Yun Shin Chun, Claudius Conrad, Ching-Wei Tzeng, Thomas Aloia, Jean-Nicolas Vauthey
Surgical Oncology, MD Anderson Cancer Center, Houston, TX
Objective: To evaluate the impact of repeat surgical resection for recurrent disease after completion of two-stage hepatectomy (TSH) for bilateral colorectal liver metastases (CLM) and the prognostic role of RAS mutation status in this cohort.
Background: Two-stage hepatectomy is associated with a high rate of recurrence. There is no established treatment approach for recurrent disease, particularly in patients with poor prognostic factors such as RAS mutation.
Methods: 137 patients planned to undergo two-stage hepatectomy for bilateral CLM from 2004-2016. Clinicopathologic factors including RAS mutation status were evaluated and compared using univariate and multivariate analysis.
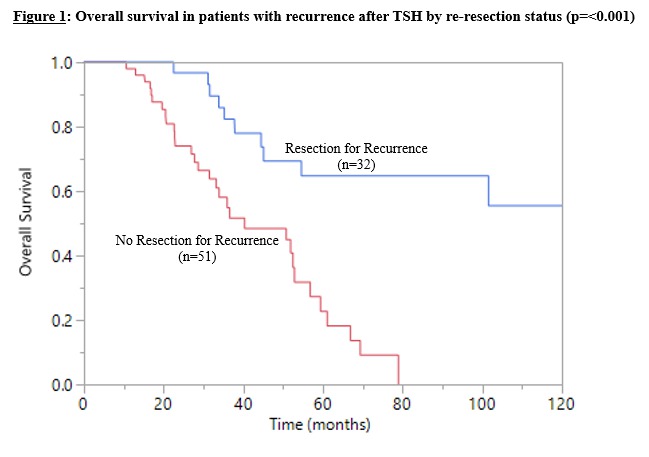
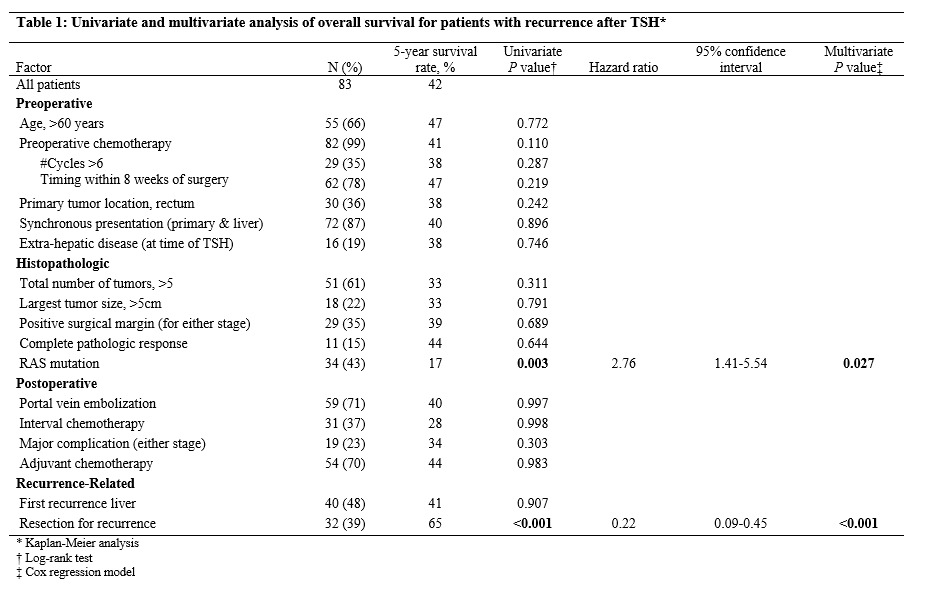
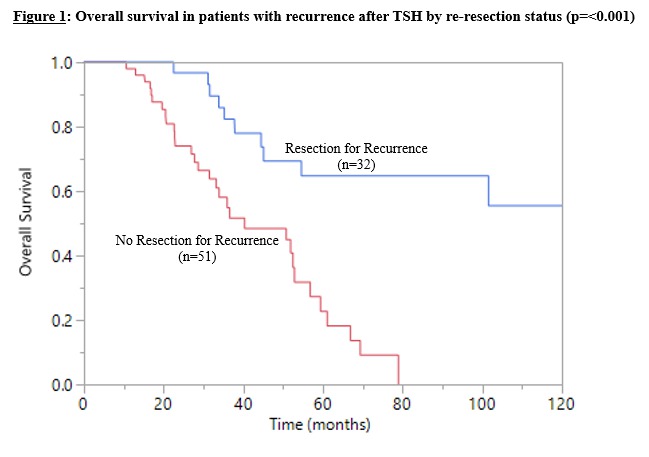
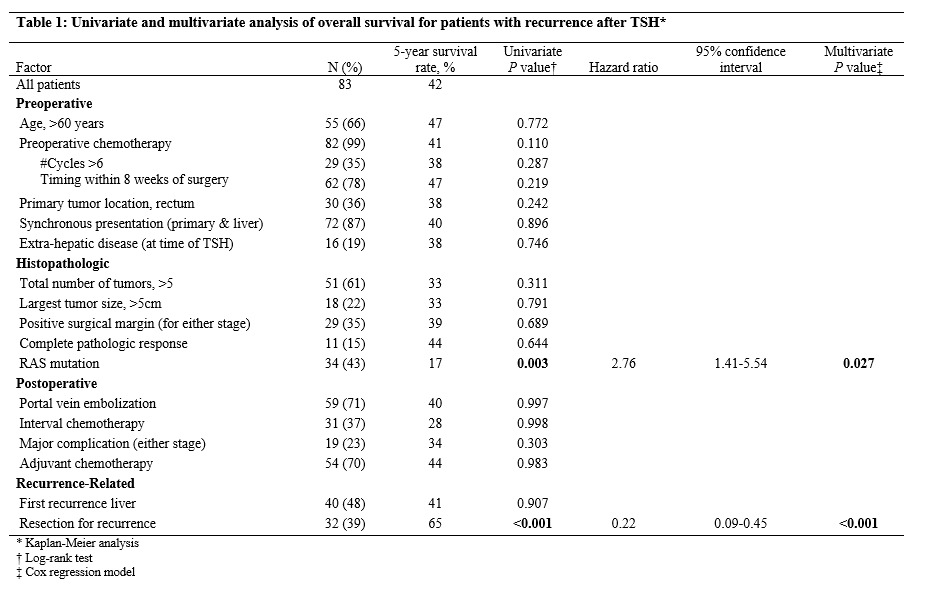
Results: 111 patients (81%) successfully completed TSH. Patients who completed the intended staged procedure had a significantly higher overall survival (OS) compared to patients who were unable to complete both stages (p<0.001). The median recurrence free survival in patients that completed TSH was 12 months. Of the 83 patients who recurred after TSH, surgical resection for recurrent disease was performed in 32 patients (39%). Resection consisted of repeat hepatectomy alone in 12 patients (38%), pulmonary resection in 7 (22%), resection of pelvic disease in 3 (9%), and combined organ site resections in 10 (31%). The median OS for this cohort was 143 months compared to 40 months for those who did not undergo re-resection (Figure 1, p<0.001). RAS mutation was also associated with significantly shorter OS (p=0.003). On multivariate analysis, both RAS mutation status and surgical resection for recurrence were independent predictors of OS (Table 1).
Conclusions: In patients who have undergone TSH for CLM, recurrence is frequent and should be treated with re-resection whenever possible. RAS wild-type patients fare particularly well with aggressive surgical management for recurrence.
Back to 2018 Program and Abstracts
|