|
Back to 2018 Program and Abstracts
POSTOPERATIVE MORBIDITY AS PREDICTOR OF EARLY RECURRENCE AND POOR SURVIVAL FOLLOWING MAJOR HEPATECTOMY FOR ADVANCED PERIHILAR CHOLANGIOCARCINOMA
Guwei Ji*, Xiangcheng Li, Xuehao Wang
Liver Transplantation Center, The First Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu, China
BACKGROUND: Postoperative complications are associated with poor prognosis and anatomic liver resection may confer survival advantages in patients with malignant liver tumors. The objective of this study was to determine the prognostic relevance of morbidity following major hepatectomy and the potential benefits of anatomic hepatectomy in perihilar cholangiocarcinoma (PHC).
METHODS: From 2008 to 2017, records of patients undergoing concomitant hemihepatectomy for advanced PHCs with curative intent were reviewed retrospectively. Severe morbidity was defined as any complication of Clavien-Dindo grade III or IV. Anatomic resection was defined as exposure of the middle hepatic vein (MHV) on the dissection plane. Predictors of survival were identified using Cox regression model. Anatomic hepatectomy and other clinical variables were analyzed as risk factors for morbidity.
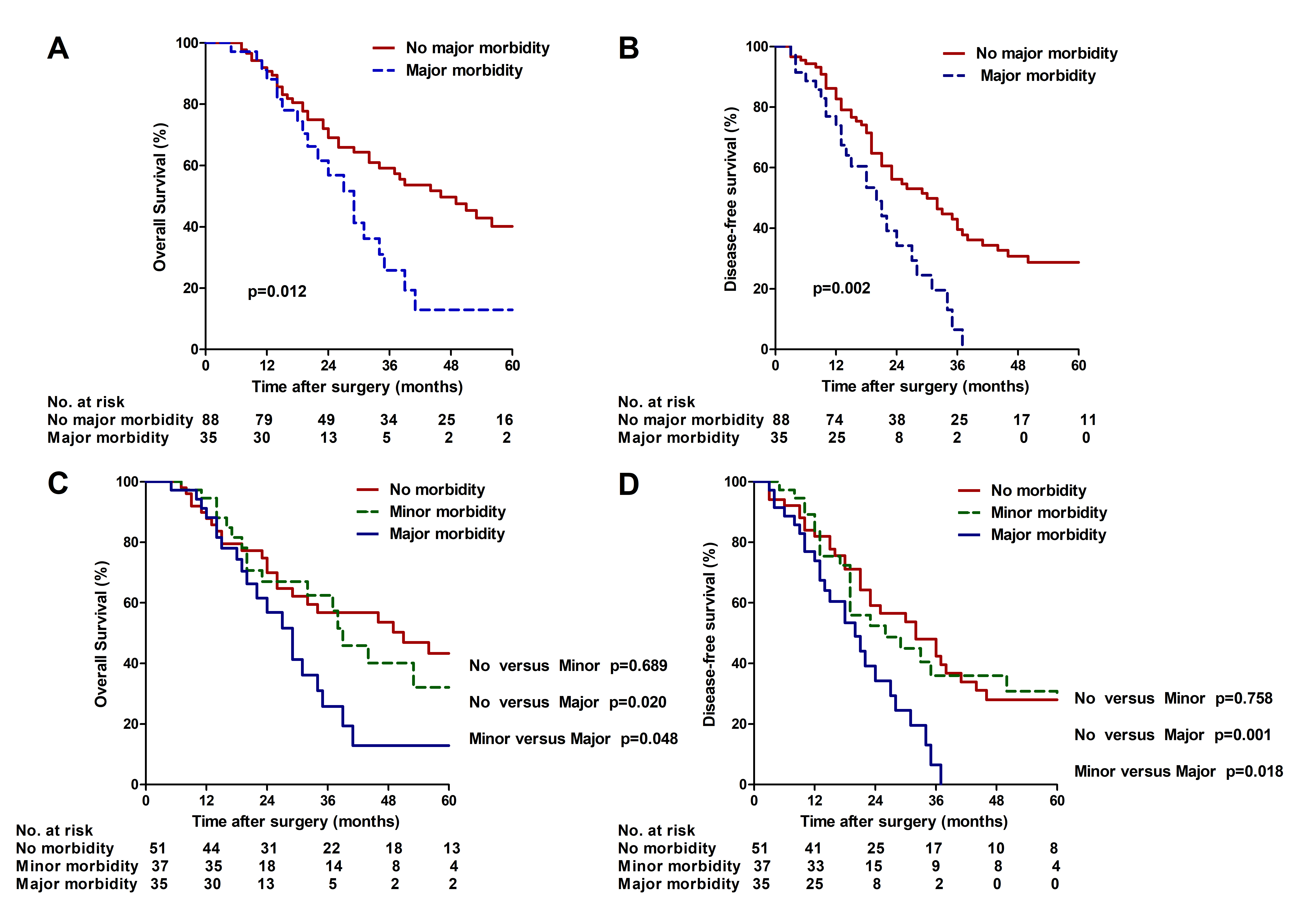
RESULTS: A total of 123 patients were enrolled and severe morbidity occurred in 36 patients (29.3%). The 5-year overall and disease-free survival for those with and without severe postoperative complications were: 12.9% versus 40.2% (P= 0.012) and 0% versus 22.0% (P=0.002), respectively. Multivariate analysis showed that severe morbidity was independently associated with early tumor recurrence (hazard ratio=1.74; P=0.046), as were elevated carcinoembryonic antigen level, positive surgical margin and nodal metastasis. Advanced age, positive surgical margin and nodal metastasis, but not severe morbidity, independently predicted shorter overall survival after curative intent resection. Subgroup analysis of patients with different severities of complications revealed similar results whereas patients with minor complications had similar survival patterns to those without complications. Advanced age, preoperative hyperbilirubinemia, anatomic hepatectomy and intraoperative transfusion were independent predictors of severe postoperative complications.
CONCLUSION: Severe morbidity was a significant predictor of early recurrence and associated with poor long-term survival after curative-intent resection for advanced PHC. Optimal preoperative preparation and MHV-oriented anatomic resection with meticulous dissection were of critical importance to minimize the risks of postoperative complications.
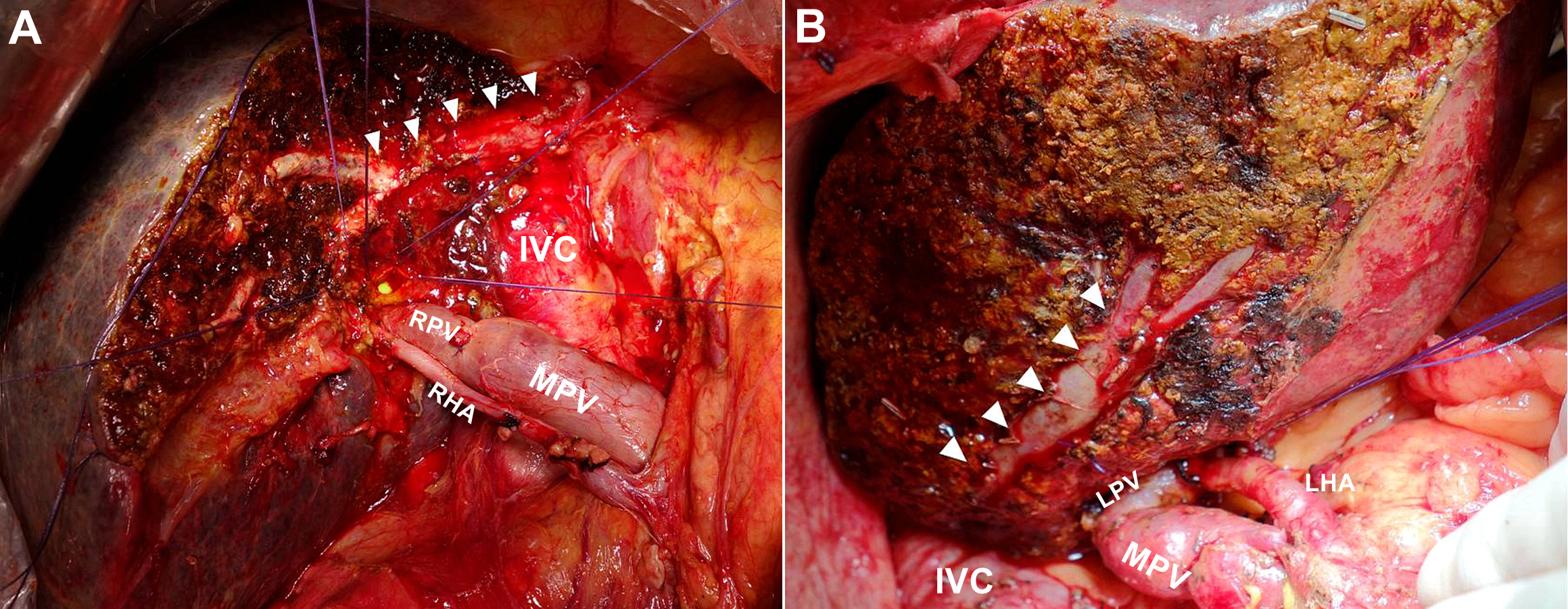
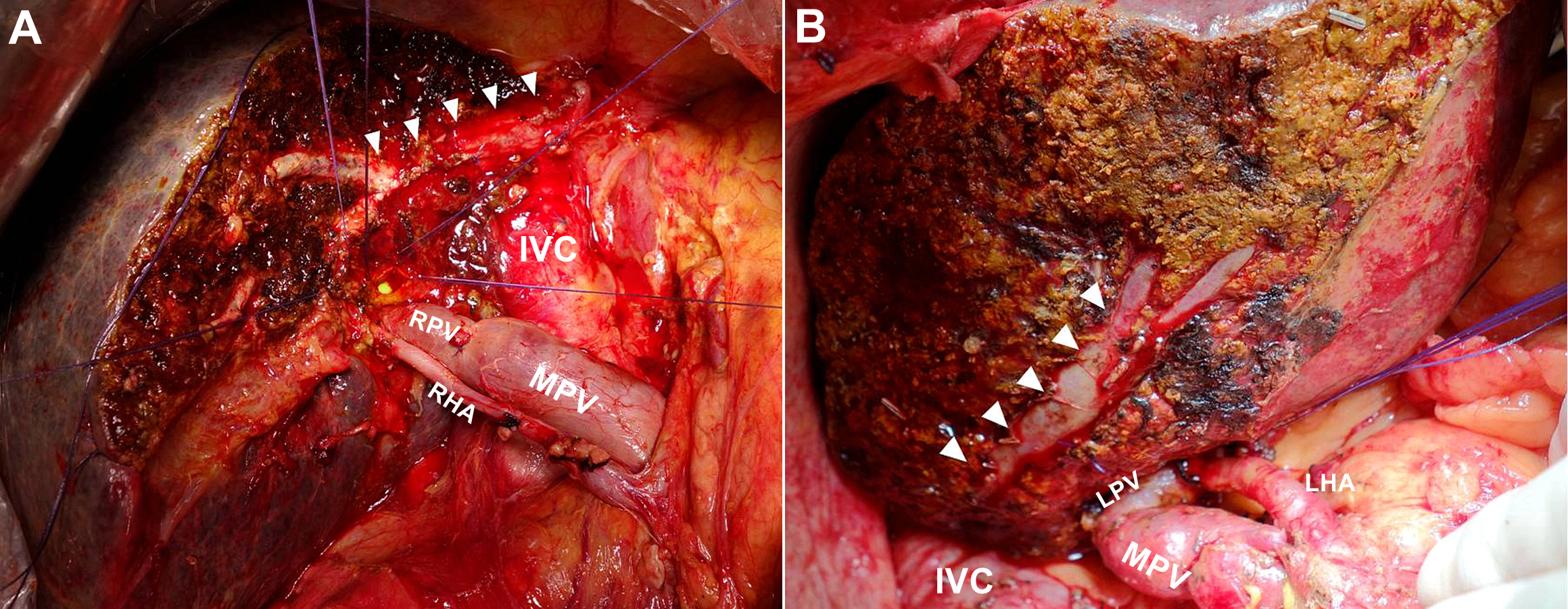
Figure 1. Anatomic left (A) and right (B) hemihepatectomy for radical resection of advanced perihilar cholangiocarcinoma. The middle hepatic vein trunk (arrows) was exposed from the periphery toward the root.
RHA, right hepatic artery; RPV, right branch of the portal vein; LHA, left hepatic artery; LPV, left branch of the portal vein; IVC, inferior vena cava
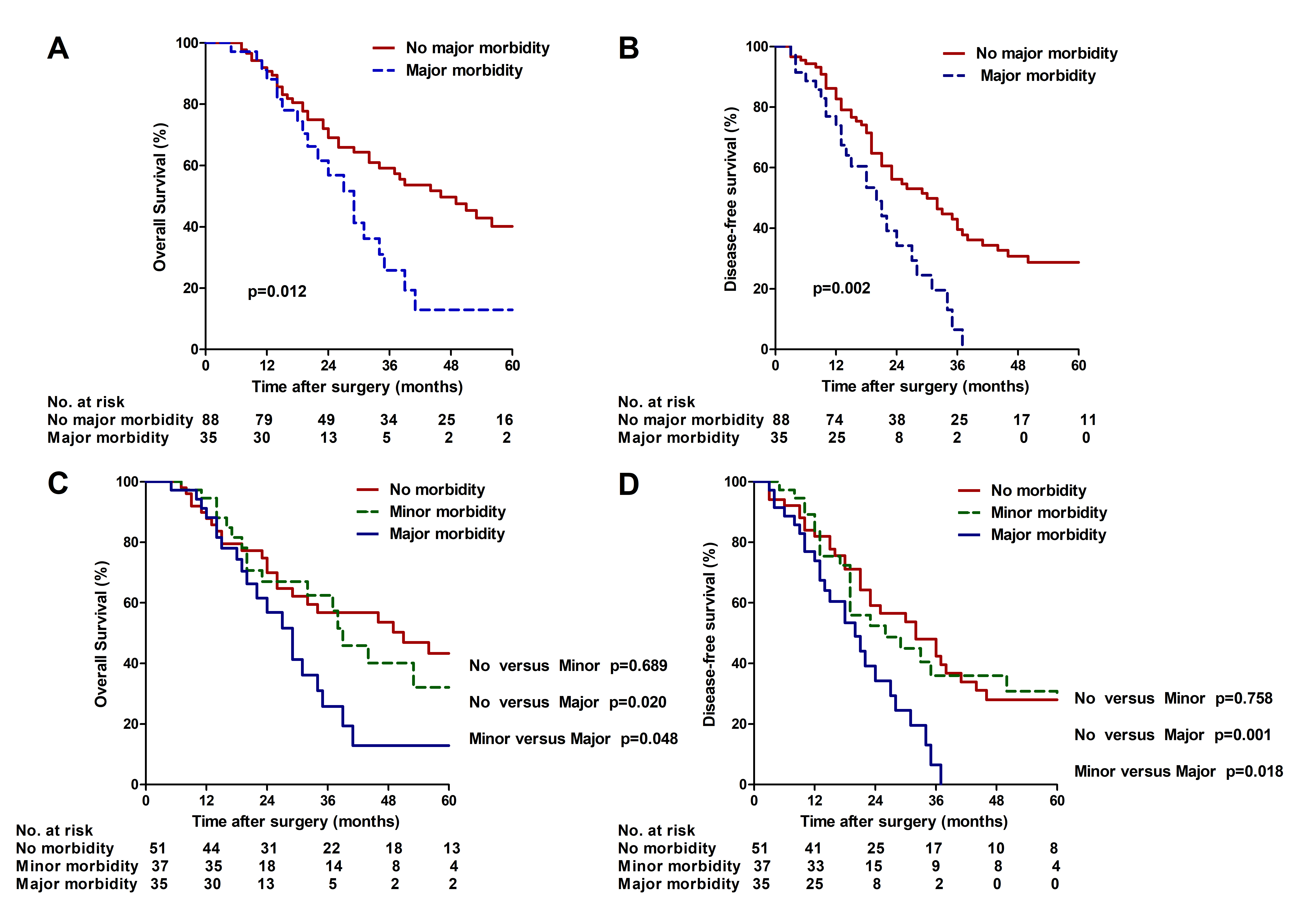
Figure 2. Kaplan-Meier survival curves for overall survival (A) and disease-free survival (B) according to the presence and absence of severe morbidity. Overall survival (C) and disease-free survival (D) stratified by severity of postoperative complications according to Clavien-Dindo classification.
Back to 2018 Program and Abstracts
|