|
Back to 2018 Program and Abstracts
THE INFLUENCE OF HOSPITAL VOLUME AND PAYOR STATUS ON 5-YEAR OUTCOMES IN PATIENTS UNDERGOING LAPAROSCOPIC VS OPEN BILATERAL INGUINAL HERNIA REPAIR
Hien Nguyen, Ambar Mehta*, Joseph K. Canner, Gina Adrales, Thomas Magnuson, Michael Schweitzer, Alisa Coker, Alex Blair
Johns Hopkins, Baltimore, MD
Background:While previous studies have compared laparoscopic versus open repairs for unilateral inguinal hernias, few have examined these operative techniques among bilateral inguinal hernias. In this statewide study, we assessed (1) the utilization of laparoscopic repairs for bilateral inguinal hernias, (2) both short-term and long-term outcomes, and (3) predictors of adverse outcomes.
Methods:Using the 2005-2011 California State Ambulatory Surgical and Emergency Department Database, we identified patients undergoing bilateral inguinal hernia repairs who did not have any contraindications to underging laparoscopic surgery. We compared 30-day postoperative emergency department (ED) visits and 5-year reoperative rates between laparoscopic and open repairs. We assessed predictors of adverse outcomes among low-volume and high volume ambulatory surgical centers (ASCs), which were identified as those that performed at least 10 open and 10 laparoscopic bilateral inguinal hernia repairs annually to those that performed at least 50 open and 50 laparoscopic cases, respectively. All analyses adjusted for the following: patient age, gender, race and ethnicity, payer, number of comorbidities, center volume (defined by tertiles), and clustering by centers.
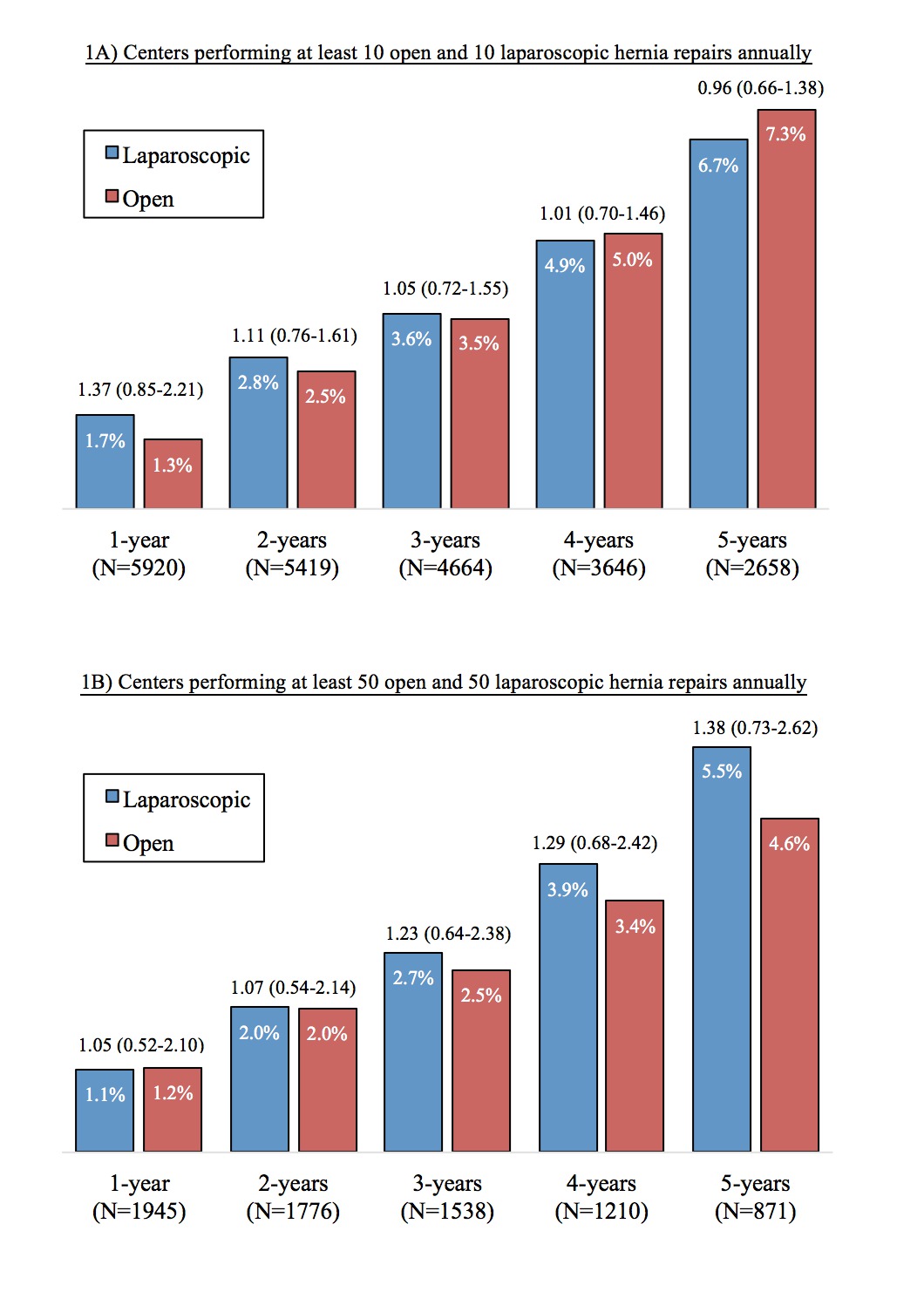
Results:We identified 6559 patients undergoing elective bilateral inguinal hernia repairs (open:30.6%, laparoscopic:69.4%). The 30-day post op ED visit rate was 4.4% (open: 5.3%, laparoscopic: 3.9%); the most common causes were urinary or gastrointestinal symptoms. Re-operative rates ranged from 1.6% within one-year to 6.9% within five-years. After adjustment, both laparoscopic and open repairs had similar 30-day ED visits (aOR 0.79 [95%-CI 0.60-1.05],(Table 1) and rates of re-operation within one-year (aOR 1.37 [0.85-2.21]) to five-years (aOR 0.96 [0.66-1.38]) Comparison of low vs high ASC volume did not show significant difference in postoperative ED visits or rates of re-operation within up to five years(Figure 1). Relative to private insurance, both self-pay (aOR 1.76 [1.05-2.97]) and Medicaid (aOR 3.09 [1.23-7.80]) insurance status had increased adjusted odds of five-year reoperation rates and are more likely to undergo an open repair, Medicaid (aOR 1.91 [1.38-2.64]) and Medicare (aOR 1.25 [1.02-1.53]).
Discussion:Among patients with bilateral inguinal hernias who were eligible for a laparoscopic repair, almost one-third underwent an open repair. Patients with Medicaid insurance had a higher association with undergoing an open repair and re-operation within 5-years. Laparoscopic repairs had similar rates of 30-day postoperative ED visits compared to open. Five-year re-operation rates are similar between laparoscopic and open cases, and between ASC's that have lower versus higher yearly volumes. Therefore, laparoscopic repair is safe for patients with bilateral inguinal hernias, even at low volume centers.
Emergency department visits within 30-days of bilateral inguinal hernia repairs.
| | Total | Open Repair | Laparoscopic Repair | Adjusted P-value | | Number | 6519 | 2003 | 4516 | -- | | 30-day ED Visit | 284 (4.4%) | 107 (5.3%) | 177 (3.9%) | 0.10 | | Urinary symptoms | 78 (1.2%) | 16 (0.8%) | 62 (1.4%) | 0.06 | | GI symptoms | 70 (1.1%) | 32 (1.6%) | 38 (0.8%) | 0.02 | | Chest pain or SOB | 11 (0.2%) | 2 (0.1%) | 9 (0.2%) | N/A | | Fever or infection | 10 (0.2%) | 3 (0.2%) | 7 (0.2%) | N/A |
SOB = shortness of breath 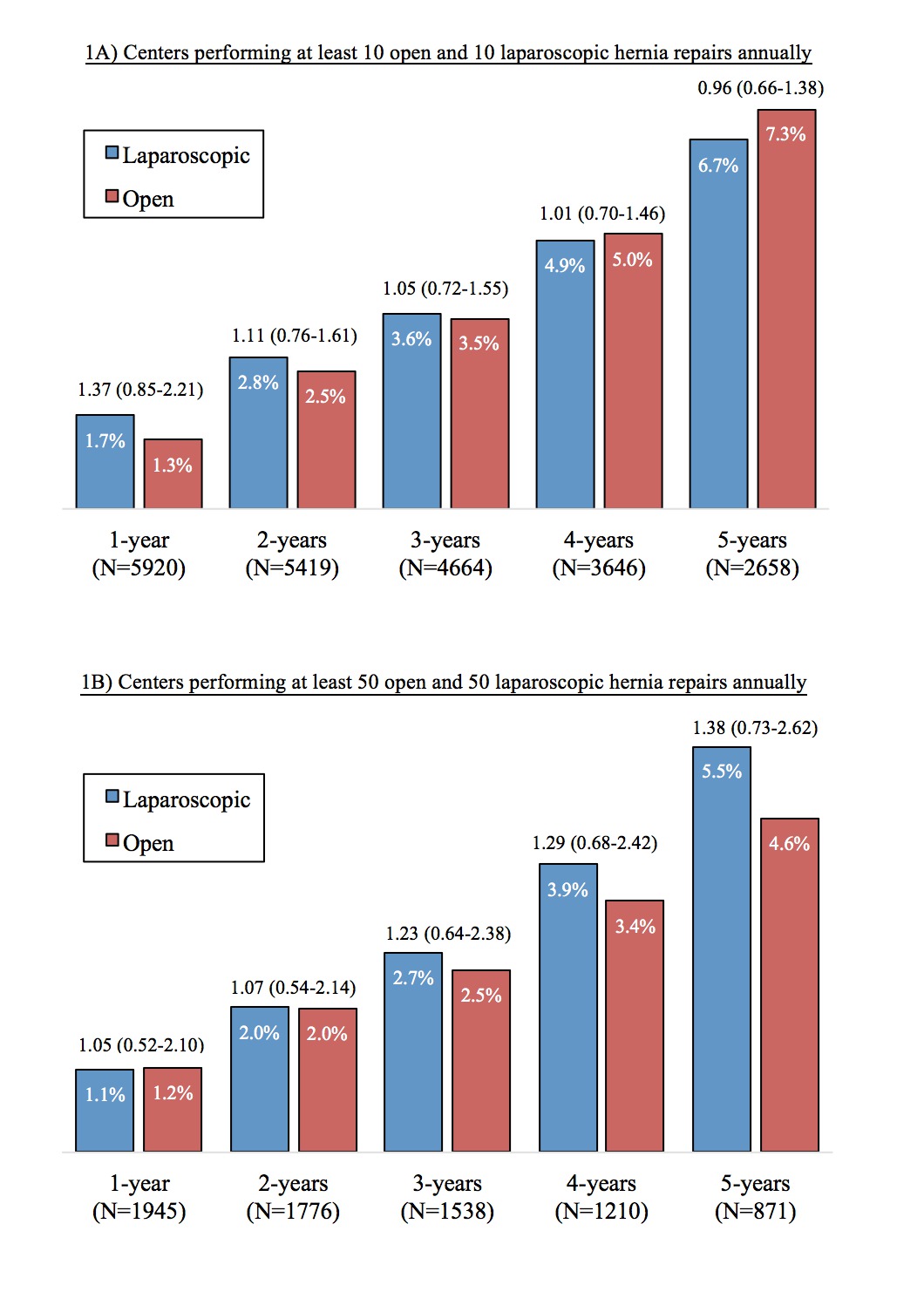 Figure 1: Yearly recurrence rates of laparoscopic versus open repairs of bilateral inguinal hernias. Figure 1: Yearly recurrence rates of laparoscopic versus open repairs of bilateral inguinal hernias. After adjustment, laparoscopic repairs were not associated with increased rates of recurrence within five years relative to open repairs (adjusted odds ratios shown above bars) at either low-volume (1A) or high-volume centers (1B).
Back to 2018 Program and Abstracts
|