|
Back to 2018 Program and Abstracts
SURGERY DURING HOSPITALIZATION FOR A CHRONIC ULCERATIVE COLITIS FLARE: SHOULD POUCH FORMATION BE CONSIDERED?
Nicholas P. McKenna*1, Katherine Bews1, Amy L. Lightner2, Kellie L. Mathis2, Elizabeth B. Habermann1
1Surgery, Mayo Clinic, Rochester, MN; 2Colon and Rectal Surgery, Mayo Clinic, Rochester, MN
Background: Roughly 25% of patients with chronic ulcerative colitis (CUC) will require hospitalization for an acute flare of their disease, and up to 20% of these patients will require colectomy during the same hospitalization. There is limited evidence to guide decision making on the safety of ileal pouch anal anastomosis (IPAA) formation in patients requiring surgery during admission for an acute flare. We sought to determine the impact of semi-urgent status on major morbidity at the time of total proctocolectomy (TPC) with IPAA using the American College of Surgeons National Quality Surgical Improvement Project (ACS-NSQIP) database.
Methods: The ACS-NSQIP multicenter database was queried for patients with a diagnosis of CUC undergoing either elective TPC with IPAA (surgery the day of admission), semi-urgent TPC with IPAA during an admission for a CUC flare (defined as hospitalization >48 hours prior to surgery), or semi-urgent subtotal colectomy (STC) during an admission for a CUC flare (defined as hospitalization >48 hours prior to surgery) between 2005 and 2015. Patients with an ASA score greater than III, in septic shock pre-operatively, or who underwent an emergent operation were excluded. The association of semi-urgent status with major morbidity was assessed using univariate comparisons and multivariable logistic regression.
Results: 5950 patients met inclusion criteria (elective TPC with IPAA=4231, semi-urgent TPC with IPAA=193, semi-urgent STC=1526). Patients who underwent a semi-urgent TPC with IPAA were more often malnourished (albumin < 3.5 g/dL, 71% vs 16%), anemic (hematocrit < 30%, 31% vs 5%), and on immunosuppressive medications (43% vs 32%) (all p<0.01) than those who had an elective TPC with IPAA. Patients undergoing semi-urgent STC were more often malnourished (79% vs 71%) and anemic (38% vs 31%) than those undergoing semi-urgent TPC with IPAA (both p<0.05), but outpatient immunosuppressant use (47% vs 43%) did not differ (p>0.05).
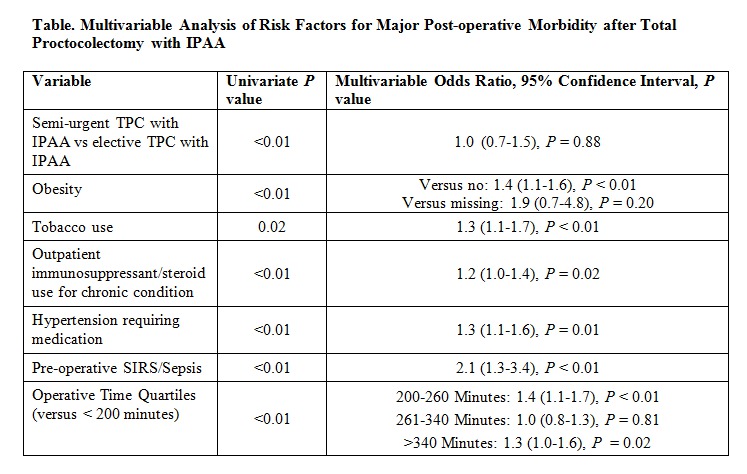
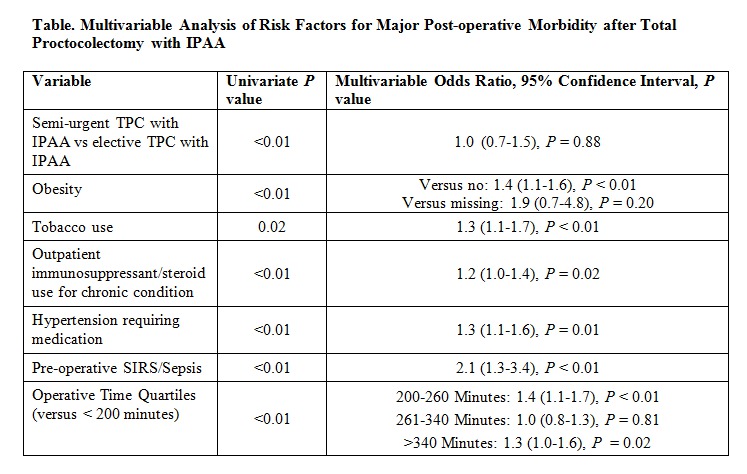
Inpatient TPC with IPAA was associated with a higher rate of major morbidity than elective outpatient TPC with IPAA (27% vs 19%, p=0.01). However, on multivariable analysis, semi-urgent surgery was not predictive of major morbidity (adjusted odds ratio [AOR], 1.0; 95% confidence interval [CI], 0.7-1.5), while other previously identified risk factors were independently associated with increased morbidity (Table). Major morbidity did not differ between semi-urgent TPC with IPAA and semi-urgent STC (27% vs 24%, p=0.53; AOR, 1.2; 95% CI, 0.8-1.7).
Conclusions: Pouch formation in the semi-urgent setting was not independently associated with greater major morbidity than elective IPAA or semi-urgent STC. The presence of a CUC flare alone should not deter surgeons from offering an IPAA, but other well-established risk factors such as outpatient immunosuppression should be considered.
Back to 2018 Program and Abstracts
|