|
 |
Back to 2018 Program and Abstracts
THERAPY REFRACTORY ULCERATIVE COLITIS PATIENTS MAY BENEFIT FROM APPENDECTOMY; LONG-TERM CLINICAL RESULTS FROM A MULTICENTER PROSPECTIVE COHORT SERIES
Merel E. Stellingwerf*1, Saloomeh Sahami1, Desmond C. Winter2, Hugh E. Mulcahy2, Glen A. Doherty2, Garret Cullen2, Sean Martin2, Geert R. D'Haens3, Willem Bemelman1, Christianne J. Buskens1
1Surgery, Academic Medical Center, Amsterdam, Netherlands; 2Centre for Colorectal Disease, St Vincent's University Hospital, Dublin, Ireland; 3Department of Gastroenterology and Hepatology, Academic Medical Center, Amsterdam, Netherlands
Background: Appendectomy may lead to a reduction in relapses and need for medication in patients with ulcerative colitis (UC). However, the possibility of a placebo effect is still debated, as long-term prospective data are lacking. The aim of this study was to analyze the effect of an appendectomy on the clinical course of therapy refractory UC patients.
Methods: In this observational prospective cohort study, a consecutive series of therapy refractory UC patients referred for proctocolectomy between November 2012 and June 2015 were counseled to undergo laparoscopic appendectomy first. Primary endpoint was clinical response at 12 months and long-term follow-up (>2 years), defined as a decrease of ≥3 points in the partial Mayo ranging from 0-9. Secondary endpoints were failure (colectomy or start of new, mostly experimental medication), endoscopic remission (endoscopic Mayo score ≥1), changes in IBDQ (range 32-224), and a patient rated 'global change' question ("Since your operation, have your UC symptoms improved overall?"?). To assess clinical relevance of changes in the IBDQ, the clinical minimally important difference (MID) in IBDQ was calculated from the difference in IBDQ change scores of the patients answering "yes"? and "no"? to the global change question. Statistical differences were analyzed using mixed-models analysis for repeated measures applying a random-effects model.
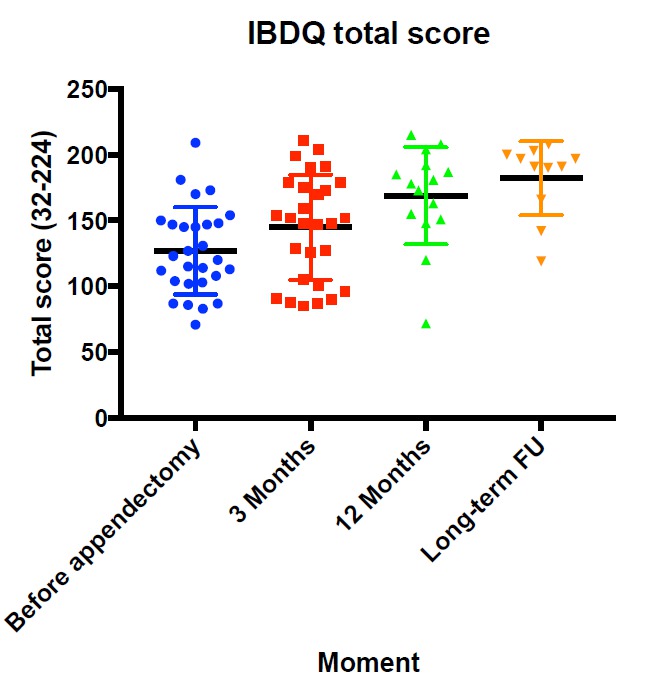
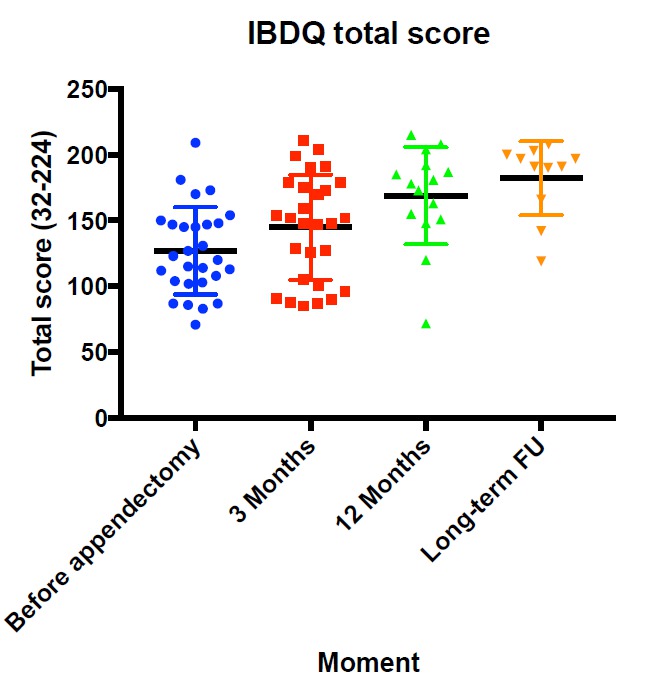
Results: In total, 28 patients (46% female, 10 using steroids) with a median age of 41 (IQR, 33-48) underwent appendectomy with a median preoperative partial Mayo score of 7 (IQR, 6-8). The mean baseline IBDQ was 127 (95%CI 113-141).
After 12 months, 12/26 (46%) patients had a clinical response, none using steroids. Of those with a response, 3/12 refused endoscopy and 5/12 were in endoscopic remission. A total of 10 patients failed (6x colectomy, 4x experimental medication). For the remaining patients, the IBDQ significantly improved to mean 161 (95%CI 144-177; p<0.001).
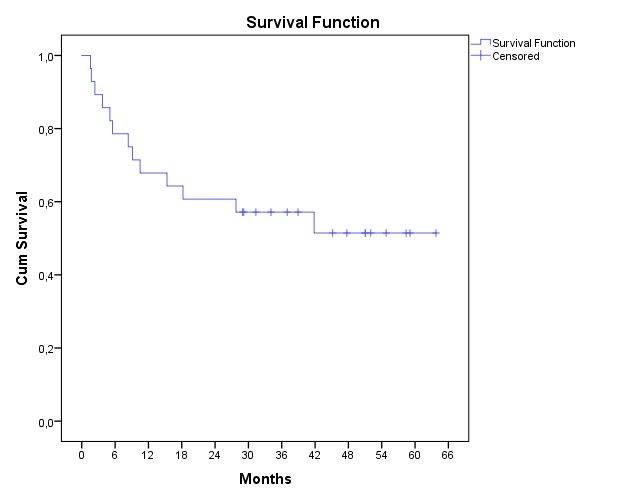
Long-term data were available for 27/28 patients. After median follow-up of 4 years (range 2-5) another 3 patients failed (in total 9x colectomy, 4x experimental medication; Figure 1). Thirteen of the remaining 14 patients had clinical response (4 using steroids) of whom 6 were in endoscopic remission (endoscopy data of 3 patients is pending). The IBDQ was further improved to mean 169 (95%CI 151-188; p<0.001; Figure 2). Overall, 77% of the patients answered "yes" to the global change question, the MID for improvement of the IBDQ was 26 points resulting in a clinical benefit for 75% of the patients.
Conclusion: After long-term follow-up, appendectomy resulted in a clinical response in at least 48% of therapy refractory UC patients of whom 46% were in endoscopic remission. An appendectomy could be beneficial in this patient group, as a long-term (endoscopic) placebo effect seems unlikely.
Figure 1. Kaplan-Meier survival curve of failure
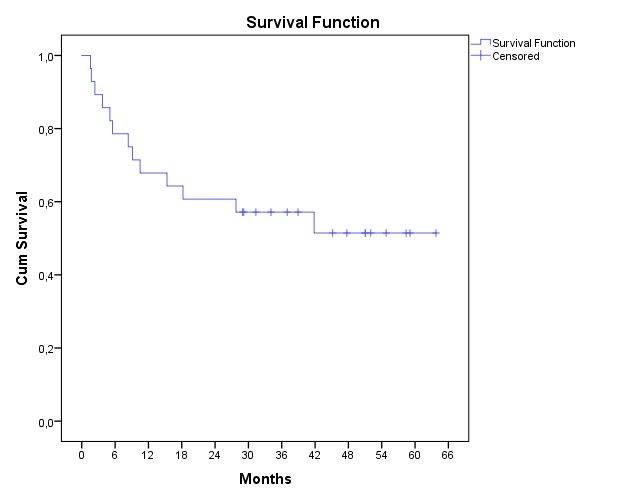
Figure 2. Scatter dot plot of total IBDQ scores
Back to 2018 Program and Abstracts
|