|
 |
Back to 2018 Program and Abstracts
ABLATION VERSUS HEPATECTOMY FOR EARLY-STAGE HEPATOCELLULAR CARCINOMA: A MATCHED NATIONWIDE REVIEW
Susanna W. de Geus*2, Gyulnara Kasumova2, Tara S. Kent1, Sing Chau Ng2, David McAneny2, Teviah Sachs2, Jennifer Tseng2
1Surgical Oncology, Beth Israel Deaconess Medical Center, Boston, MA; 2Surgery, Boston Medical Center, Boston, MA
Background: Ablation (ABL), surgical resection (RXN), and transplantation (TXP) are considered first-line treatment strategies for hepatocellular carcinoma (HCC). ABL offers the opportunity to circumvent the dependency on scarce donor organs, considerable surgical mortality, and the lengthy hospital stay that accompany RXN and TXP. Previous studies have reported ambiguous results regarding the efficacy of ABL and a wide variety of tumor size cutoff have been proposed, ranging from 20 mm to up to 50 mm. This study compares survival outcomes between patients that underwent RXN, ABL, and TXP for HCC using nationwide data
Methods: Patients with HCC of £ 50 mm that underwent RXN, ABL, or TXP were identified from the National Cancer Database (2004-2014). Four cohorts were created based on tumor size: £ 20 mm, 21-30 mm, 31-40 mm, and 41-50 mm. To prevent selection bias propensity score models for the odds of receiving RXN were created. Patients were matched on propensity score. Survival analysis was performed using the Kaplan-Meier method.
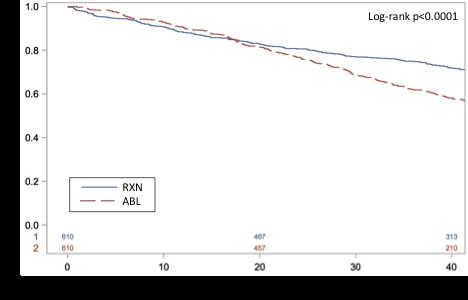
Results: In the overall cohort, 18.8% (n=2,931), 34.5% (n=5,366), and 46.7% (n=7,265) of patients underwent RXN, ABL, and TXP, respectively. 32.5% (n=5,062) were diagnosed with HCC of £ 20 mm, 35.3% (n=5,496) with HCC of 21-30 mm, 20.3% (n=3,158) with HCC of 31-40 mm, and 11.9% (n=1,846) with HCC of 41-50 mm. After matching within size groups, patients with HCC of £ 20 mm who underwent ABL initially experienced remote survival benefit; however, after approximately 20 months the curves cross and RXN becomes associated with long-term survival compared to ABL (median survival, 113.5 vs. 53.7 months; p<0.0001). Patients with HCC of 21-30 mm who underwent ABL had favorable survival for the first 10 months approximately, but thereafter RXN was associated with improved survival compared to patients who underwent RFA (median survival, 72.3 vs. 42.1 months; p<0.0001). RXN also demonstrated higher survival compared to ABL in patients with HCC of 31-40 mm (median survival, 56.6 vs. 31.9 months; p<0.0001) and 41-50 mm (median survival, 46.6 vs. 25.3 months; p<0.0001). TXP was associated with superior survival compared to RXN in patients with HCC of £ 20 mm (median survival, not reached vs. 113.5 months; p<0.0001), 21-30 mm (median survival, 142.0 vs. 73.1 months; p<0.0001), 31-40 mm (median survival, 117.4 vs. 59.6 months; p<0.0001), and 41-50 mm (median survival, 116.9 vs. 51.8 months; p<0.0001)
Conclusion: TXP demonstrated superior survival outcomes for all tumor sizes; however, this study did not account for patients that progressed while awaiting TXP. RFA may provide a feasible bridging strategy until TXP for small HCC; however, RXN is preferable in terms of long-term survival, even for small HCC.
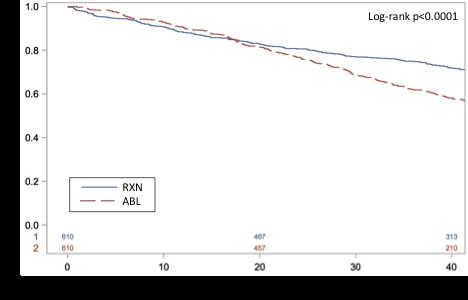
Kaplan-Meier curve for overall survival comparing ablation (ABL) to surgical resection (RXN) after matching in hepatocellular carcinoma of less than 20 mm
Back to 2018 Program and Abstracts
|