|
 |
Back to 2018 Program and Abstracts
10 YEAR EXPERIENCE WITH GALLBLADDER CARCINOMA IN A HIGH VOLUME CENTER: PATHOLOGIC VARIABLES, SURVIVAL AND PATTERNS OF RECURRENCE
Nathan M. Bolton*1, Daniel Solomon1, Natasha Leigh2, Daniela Feingold1, Deepa Magge2,1, Benjamin Golas2,1, Daniel Labow2,1, Umut Sarpel1
1Surgery, Mount Sinai, New York, NY; 2Surgery, Mount Sinai St. Luke's, NY, NY
Introduction
The rare diagnosis of gallbladder carcinoma (GBC) carries a poor prognosis, with overall 5-year survival between 5-13% and surgical resection the only potentially curative treatment option.
Methods
We retrospectively analyzed all patients with GBC who underwent resection for cure by specialized hepatobiliary surgeons in our health system from 2007-2017. Baseline demographics were compared between patients stratified by final stage and analyses were performed on baseline, clinical, and pathologic variables to identify differences in overall (OS) and disease free survival (DFS).
Results
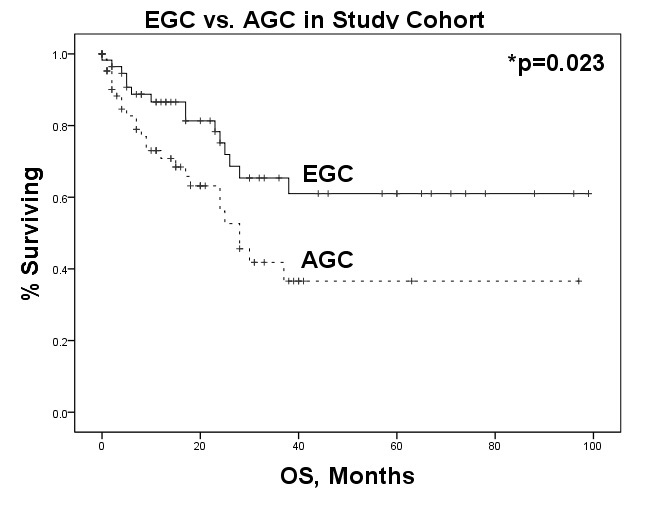
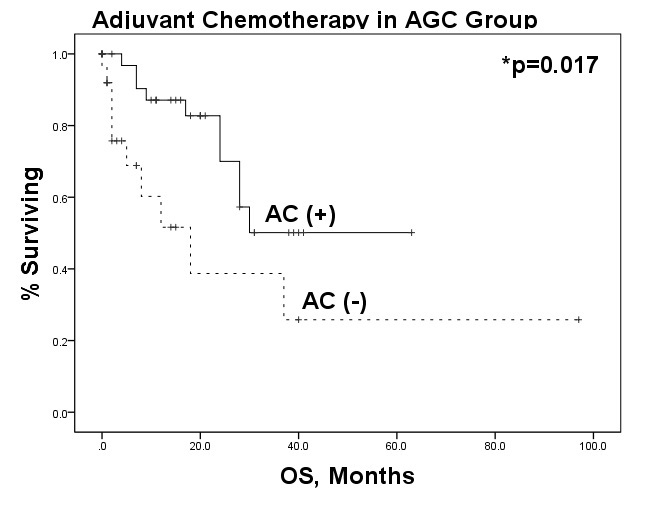
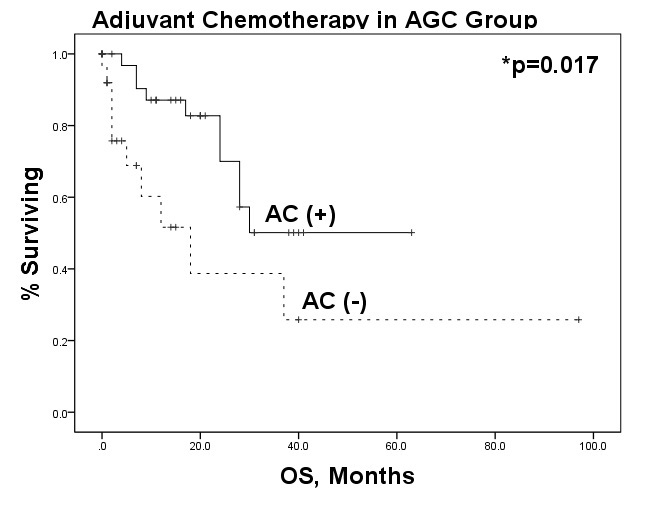
127 patients underwent resection for non-metastatic GC during the above time period. Cases were divided into early gallbladder cancer (EGC) (AJCC Stage I/II, n=58) and advanced gallbladder cancer (AGC) (AJCC Stage III/IVa, n=68). Baseline characteristics were compared between the two groups. Overall R0 resection was 80.9%. More patients in the EGC were R0 (98.3% v 66.2%, p<0.001). AGC were less likely to be found incidentally (50.0% v 70.7%, p=0.02), had higher incidence of perineural invasion (PNI)(50% v 17%, p<0.001) and lymphovascular invasion (LVI)(50% vs 17%, p<0.001), and were more likely exhibit grade 2/3 differentiation (91.2% v 74.2%, p=0.01). They were also more likely to receive adjuvant chemotherapy (47.1% v 17.2%, p<0.001) and radiotherapy (22.1% v 8.6%, p=0.04). Kaplan-Meier curve shows expected poorer OS in AGC (median OS 25 mos AGC v not reached EGC, p=0.02) with a median followup of 38 mos (fig 1). On Cox regression in the AGC group incidental diagnosis (HR 0.307(0.131, 0.719),p=0.007), young age (HR 1.035(1.004, 1.068),p=0.03), T-status (HR 2.444(1.320, 4.528), p=0.004), adjuvant chemotherapy (AC) (HR 0.356(0.146, 0.871), p=0.02), and liver resection (HR 0.4(0.182, 0.879), p=0.02) were associated with improved OS. LVI (HR 2.800(1.016, 7.719), p=0.05), 30-day complications (HR 3.120(1.014, 9.604), p=0.05) and readmissions (HR 4.117(1.388, 12.217), p=0.01) were associated with poorer OS. On multivariate regression only AC (HR 0.178(0.057, 0.558), p=0.003) and incidental diagnosis (HR 0.155(0.049, 0.489), p=0.001) remained protective. No specific patterns were unveiled in terms of locoregional or distant recurrence (50% v 50%, p=0.462). There was no significant difference in recurrence site based on stage, LVI, or PNI. On Cox univariate regression the only predictor of reccurence was AC (HR 0.327(0.111, 0.969), p=0.044).
Conclusions
Although generally carrying a poor prognosis, our data revealed that at a high volume center GBC had a median OS of 25 months in more advanced stage patients, with the most significant predictors of survival being incidental diagnosis and the addition of AC. Pathologic features, including LVI and PNI, did not predict site of recurrence. Further randomized trials are necessary to guide therapy in this rare disease.
Fig 1. Overall Survival, EGC vs AGC
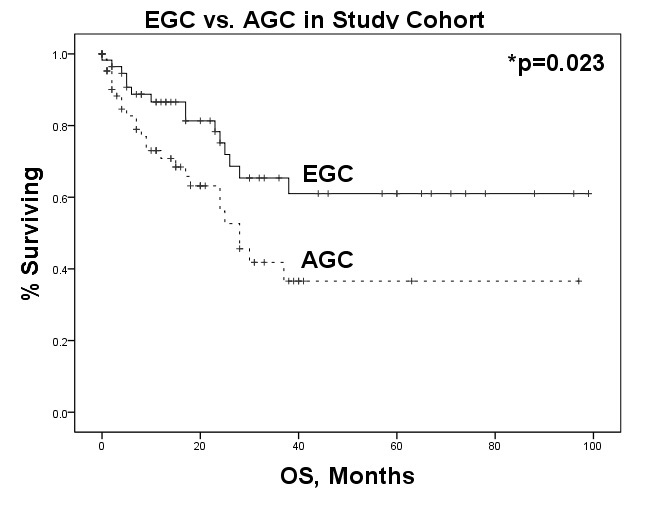
Fig 2. Effect of Adjuvant Chemotherapy in Advanced Gallbladder Cancer
Back to 2018 Program and Abstracts
|