|
Back to 2018 Program and Abstracts
SYSTEMATIC TREATMENT OF SLEEVE GASTRECTOMY STENOSIS WITH HYDROSTATIC AND PNEUMATIC BALLOON DILATION IS SAFE AND EFFECTIVE
Pichamol Jirapinyo*1, Wasif M. Abidi2, Christopher C. Thompson1
1Brigham & Women's Hospital, Boston, MA; 2Gastroenterology, Baylor College of Medicine, Houston, TX
Background: Sleeve gastrectomy is the most commonly performed bariatric surgery in the U.S. Sleeve gastrectomy stenosis (SGS) is a common complication after sleeve gastrectomy. Management includes conservative therapy, endoscopic therapy (dilation or stent placement) and surgical revision.
Aim: To assess the safety and efficacy of a protocol-based endoscopic treatment algorithm for SGS.
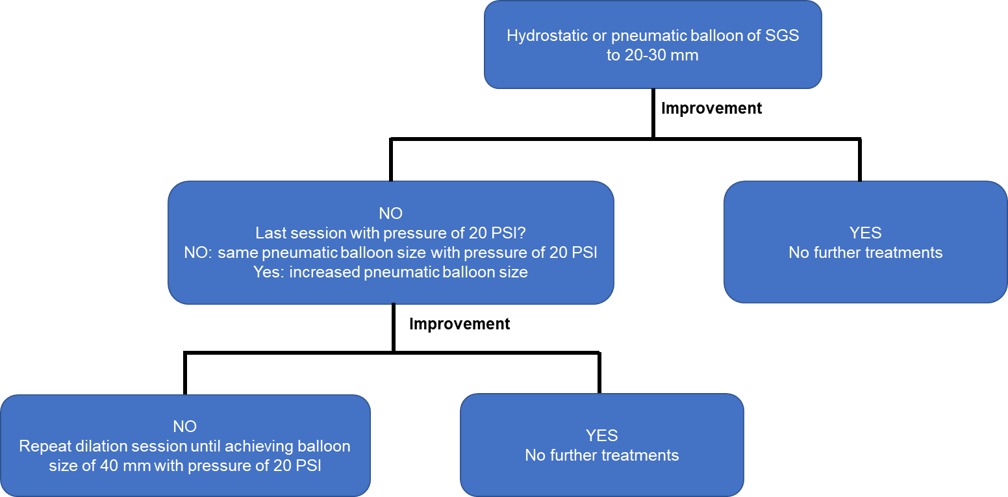
Methods: This was a retrospective study of prospectively collected data of patients who underwent endoscopic treatment for SGS. Patients were initially treated with balloon dilation of their SGS using a hydrostatic balloon to 20 mm or a pneumatic balloon to 30 mm. If the patient did not improve, they were treated with successive pneumatic balloon dilations of the SGS up to 40 mm (Figure 1). Successive treatments maintained the same balloon size if maximal pressure had not been achieved on the prior session, and advanced to the next balloon size only if maximal pressure had been achieved, to reduce the risk of perforation. Treatments were repeated every 2-4 weeks. Treatments were discontinued if the patient reported durable resolution of symptoms. Primary Outcome: Clinical success was defined as improvement or resolution of symptoms that allowed the patient to avoid surgery. Failure was defined as persistence of symptoms necessitating surgical revision. Secondary Outcomes: Adverse event rate and change in weight and BMI after endoscopic dilations. All statistics were reported as mean±SD.
Results: A total of 46 SGS patients were treated with 113 dilation sessions. Average age and BMI were 45±13 years and 35.1±7.1 kg/m2. At time of presentation, patients were 5 [1,84] months post-surgery. Surgical reports were available in 19 patients. Of these, a 38 French bougie was the most commonly used (8 out of 19; 42%). Presentation symptoms included nausea/vomiting (56.5%), dysphagia (39.1%), abdominal pain (28.3%) and acid reflux (17.4%). Average dilation time was 3 [1-15] min. Primary Outcome: 37 out of 46 patients (80%) met the primary end point. Secondary Outcomes: No adverse events were encountered. At the last dilation session (90 [0,1149] days from first session), patients lost 12.9±27.3 kg and had BMI of 32.5±7.3 kg/m2 (p<0.0001). At the time of last follow-up (336 [14,1603] days], patients lost 6.6±9.1 kg and had BMI of 32.8±7.2 kg/m2 (p=0.0003).
Conclusion: Serial dilatation of SGS employing stepwise dilation with hydrostatic and pneumatic balloons up to 40 mm appears to be effective with an acceptable safety profile and low risk of weight regain. This new method may offer a less invasive and simpler alternative to surgical revision.
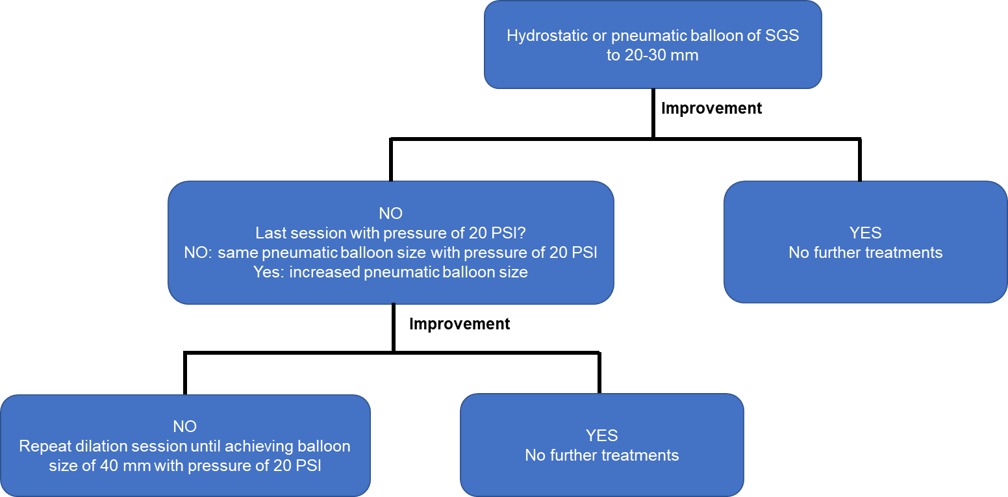
Figure 1. Algorithm for endoscopic treatment of sleeve gastrectomy stenosis
Back to 2018 Program and Abstracts
|