Back to 2018 Program and Abstracts
RELATIONSHIP BETWEEN ESOPHAGOGASTRIC JUNCTION OUTFLOW OBSTRUCTION AND DYSPHAGIA
Shaimaa Elnahas*, Takahiro Masuda, Balazs Kovacs, Sumeet Mittal
Norton Thoracic Institute, St Joesph's Hospital and Medical Center, Dignity Health, Phoenix, AZ
Background: Esophagogastric junction (EGJ) outflow obstruction (EGJOO) is a manometric diagnosis defined as lack of deglutitive lower esophageal sphincter (LES) relaxation with less than 20% simultaneous body peristalsis. Although symptoms associated with EGJOO have not been well described, dysphagia is considered to be the most prominent symptom. The aim of this study is to explore the relationship between manometric findings and dysphagia in patients diagnosed with EGJOO.
Methods: All patients undergoing high-resolution manometry (HRM) at our institution are entered into a prospectively maintained, IRB-approved database. We queried this database to identify patients diagnosed with EGJOO between Oct. 2016 and Sept. 2017. HRM studies were reanalyzed using Chicago Classification v 3.0. Patients completed a standard symptom questionnaire. Patients were divided into three groups based on dysphagia severity: Group I, no dysphagia or mild dysphagia; Group II, moderate dysphagia; and Group III, severe dysphagia. Patients with previous foregut surgery, low-quality HRM studies, or unavailable symptom questionnaires were excluded.
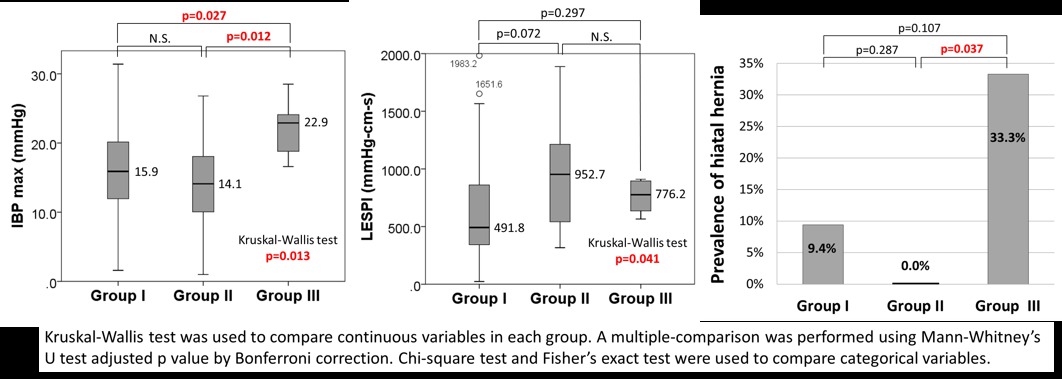
Results: In total, 1060 patients underwent HRM during the study period; of these, 119 were diagnosed with EGJOO. Patients with previous foregut surgery (n=6), low-quality HRM studies (n=8), and without symptom questionnaires (n=48) were excluded. The remaining 57 patients were categorized into the previously described groups: Group I, n=32; Group II, n=16; Group III, n=9. The mean age was 64.9 years, 37 patients were women, and the mean body mass index was 27.8 kg/m2. Six patients had manometric hiatal hernia (HH) and 13 had poor esophageal body contraction (ie, ineffective esophageal motility [ineffective peristalsis in ≥50% swallows] or fragmented peristalsis [large break in ≥50% swallows]). 30/57 patients (52.6%) reported dysphagia. No differences were observed in resting LES pressure (LESP), integrated relaxation pressure (IRP), or distal contractile integral among groups (Table 1). Groups II and III had higher LESP integral (LESPI; p=0.041). HH was most common in Group III (33.3%; p=0.033; Fig. 1). Prevalence of poor esophageal body contraction gradually increased from Group I to III (Group I: 15.6%, Group II: 25.0%, Group III: 44.4%; p=0.192). Intrabolus pressure (IBP) max was significantly higher in Group III (Group I: 15.9; Group II: 14.1, Group III: 22.9 mmHg, p=0.013).
Conclusion: More than 50% of patients with a manometric diagnosis of EGJOO report dysphagia. Elevated IBP, higher LESPI, and presence of HH were associated with higher grades of dysphagia in our cohort. Further study is needed to confirm these findings and to develop parameters for identifying patients with outflow obstruction.
Table 1. Patient Characteristics
| VARIABLE | GROUP I
No/Mild Dysphagia
n=32 | GROUP II
Moderate Dysphagia
n=16 | GROUP III
Severe Dysphagia
n=9 | p-value |
| Age, years* | 69.0 (62.5-71.0) | 63.5 (61.0-71.0) | 60.0 (46.0-66.0) | 0.228 |
| Male:Female | 14:18 | 3:13 | 3:6 | 0.221 |
| Body mass index, kg/m2 | 26.3 (23.5-30.9) | 25.4 (21.6-33.4) | 27.6 (25.7-32.2) | 0.569 |
| LESP, mmHg* | 43.9 (34.7-62.7) | 54.0 (42.7-76.5) | 58.0 (50.1-72.9) | 0.102 |
| LESPI, mmHg s cm* | 491.8 (343.2-860.7) | 952.7 (491.0-1223.5) | 776.2 (636.0-895.5) | 0.041 |
| IRP, mmHg* | 20.2 (17.1-24.7) | 23.1 (18.6-26.4) | 22.0 (17.1-26.1) | 0.526 |
| IBP max, mmHg* | 15.9 (12.0-20.2) | 14.1 (10.1-18.1) | 22.9 (18.8-24.1) | 0.013 |
| Hiatal hernia† | 3 (9.4) | 0 (0.0) | 3 (33.3) | 0.033 |
| DCI, mmHg s cm* | 1627.8 (1052.7-2994.1) | 2337.7 (921.9-4293.1) | 1308.6 (549.8-1404.0) | 0.338 |
| Esophageal body motility: Normal† | 25/32 (78.1) | 10/16 (62.5) | 5/9 (55.6) | 0.291 |
| Esophageal body motility: Poor peristalsis†‡ | 5/32 (15.6) | 4/16 (25.0) | 4/9 (44.4) | 0.192 |
| Esophageal body motility: Jackhammer esophagus† | 2/32 (6.3) | 2/16 (12.5) | 0/9 (0.0) | 0.618 |
†Values expressed are number (%) | *Values expressed are median (IQR). BMI, body mass index; LESP, lower esophageal sphincter pressure; LESPI, lower esophageal sphincter pressure integral; IRP, integrated relaxation pressure ; IBP, intrabolus pressure; DCI, distal contractile integral. ‡Poor peristalsis defined as ineffective esophageal motility or fragmented peristalsis.
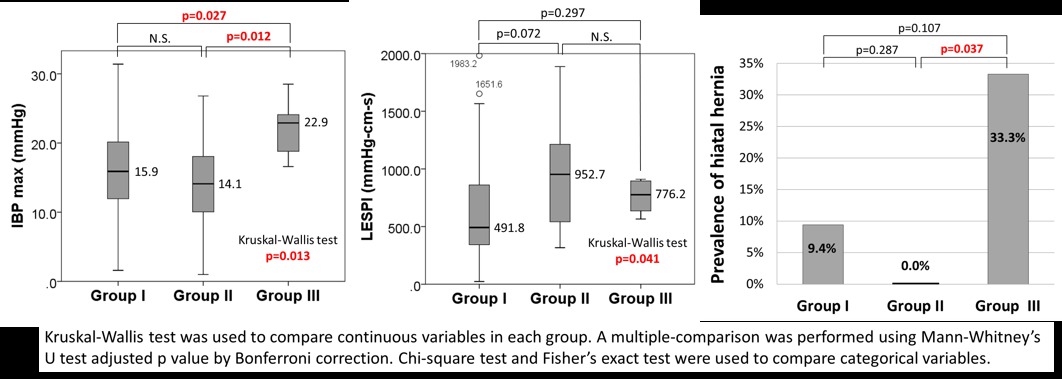
Figure 1. Differences in high-resolution manometry among study groups. (Group I: no dysphagia or mild dysphagia; Group II: moderate dysphagia; Group III: severe dysphagia.)
Back to 2018 Program and Abstracts