|
 |
Back to 2018 Program and Abstracts
SELF-EXPANDING METAL STENTS VERSUS ENDOSCOPIC VACUUM THERAPY IN THE TREATMENT OF ANASTOMOTIC LEAKS AFTER ONCOLOGICAL GASTROESOPHAGEAL SURGERY: A SINGLE-CENTER EXPERIENCE
Patrick S. Plum1, Marc Bludau1, Till Herbold2, Felix Berlth1, Hakan Alakus1, Robert Kleinert1, Christiane Bruns1, Arnulf Hölscher3, Seung-Hun Chon*1
1Department of General, Visceral and Cancer Surgery, University Hospital of Cologne, Cologne, NRW, Germany; 2Department of General, Visceral and Transplantation Surgery, RWTH Aachen University, Aachen, Germany; 3Center for Esophageal and Gastric Surgery, AGAPLESION Markus Hospital, Frankfurt am Main, Germany
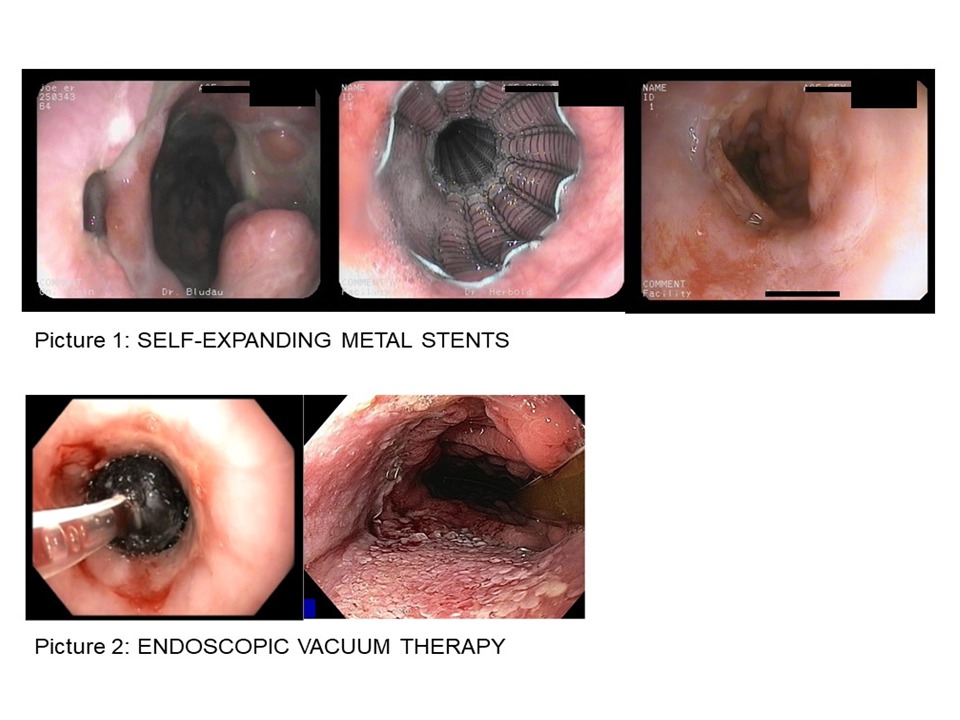
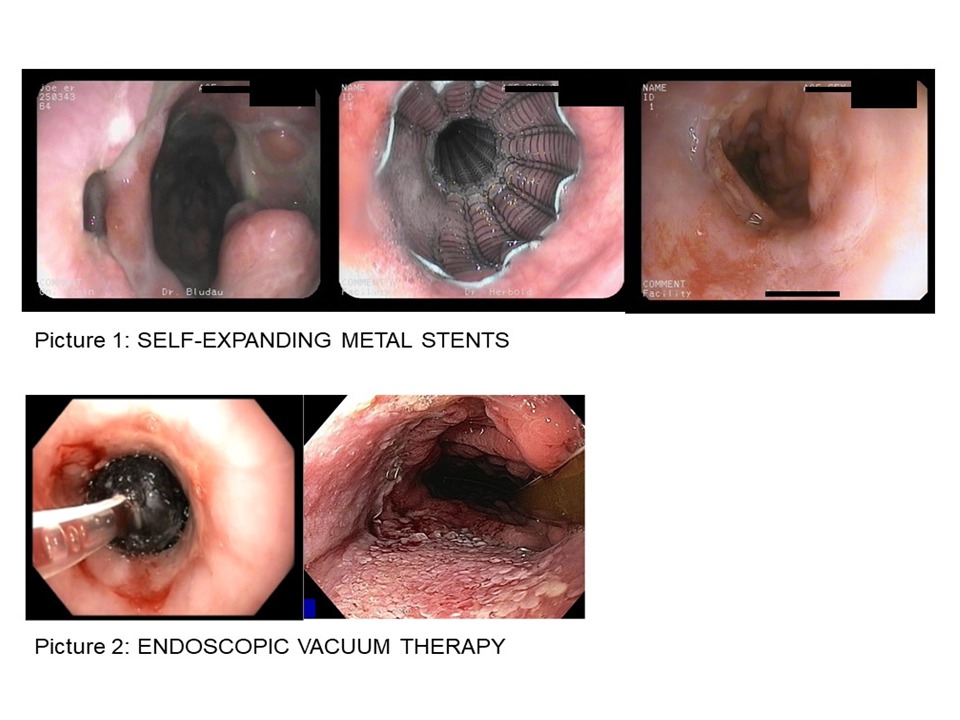
Background and Aims: Anastomotic leaks after gastroesophageal surgery are life-threatening complications. Interventional endoscopic treatment procedures, such as the implantation of self-expanding metal stents (SEMS), have been established as alternatives to surgical revision. One newer interventional therapeutic option is endoscopic vacuum treatment (EVT). This study compares the outcome and effectiveness of SEMS treatment and EVT in the management of esophageal anastomotic leaks.
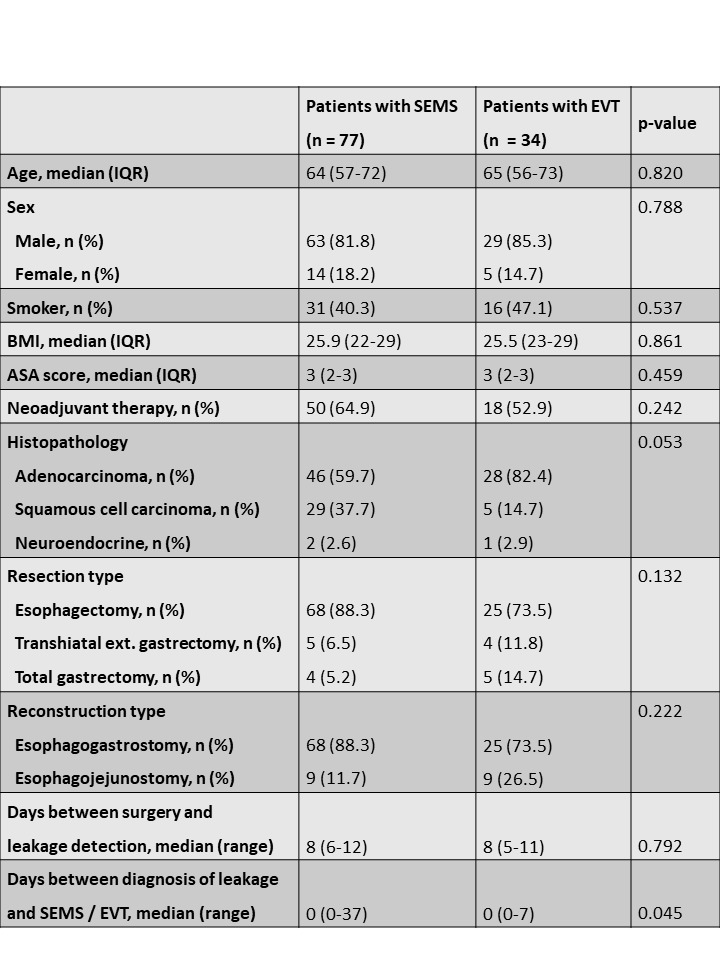
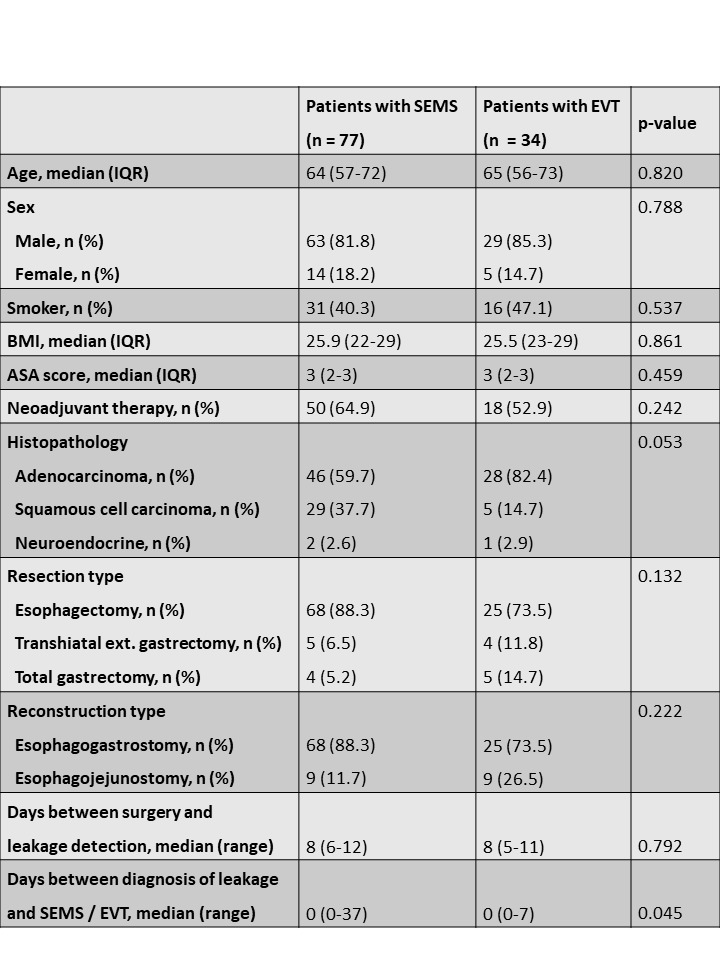
Patients and Methods: This retrospective study took place at a national referral center for tumor entities of the upper gastrointestinal tract, and the data was collected from the hospital's endoscopic and patient database. We identified all patients who were treated with SEMS or EVT for anastomotic leaks after oncological gastroesophageal surgery between 01/01/2007 and 12/31/2016. Only patients with type II leaks, according to the classification of the Esophagectomy Complications Consensus Group (ECCG), were included. In addition to the sealing success rates and intervention-related complications, we analyzed demographic characteristics, risk factors, clinical history, leak characteristics, therapy duration, and mortality.
Results: We included 111 patients who received SEMS treatment (63 male, 14 female; median age 64 years) or EVT (29 male, 5 female; median age 65 years). The overall closure rate was 70.6% (24/34) in the EVT group and 63.6% (49/77) in the SEMS group (p-value=0.477). Moreover, the intervention-related complication rate was insignificantly lower in the EVT group (8/34, 23.5%) than in the SEMS group (26/77, 26%; p-value=0.747). Patients were treated with a median of 1 stent (range 1-3) in the SEMS group compared to a median of 3 sponges (range 1-9) in the EVT group. The ICU stay ranged from 0-28 days (median 6d) for patients who received EVT and from 0-295 (median 9d) for patients who received SEMS treatment (p-value=0.001). The median therapy duration of EVT was 8.5 days (range 1-30), while the median therapy duration of SEMS treatment was 27 days (range 1-152; p-value<0.001). EVT patients were hospitalized between 19-118 days (median 37d), while patients treated with SEMS were hospitalized between 13-296 days (median 38d) (p-value=0.042). Demographic factors, comorbidities, and types of reconstruction were not predictive for the clinical success rate.
Conclusions: SEMS treatment and EVT are feasible and effective for the management of anastomotic leaks after oncological gastroesophageal surgery. According to our data, EVT not only closed leaks successfully in the majority of cases, but it also led to a shorter treatment duration, ICU stay, and hospitalization than SEMS treatment. Therefore, EVT might be more effective than SEMS treatment and should be considered in the management of esophageal anastomotic leaks.
Back to 2018 Program and Abstracts
|