|
 |
Back to 2018 Program and Abstracts
COMPARATIVE COMPLICATION RATES AFTER SLEEVE GASTRECTOMY AND GASTRIC BYPASS: AN ANALYSIS OF A NATIONAL EMPLOYER-SPONSORED INSURANCE DATABASE
Ann Y. Chung*, Paula D. Strassle, Francisco Schlottmann, Meredith Duke, Marco G. Patti, Timothy Farrell
Department of Surgery, University of North Carolina - Chapel Hill, Chapel Hill, NC
Objective: To assess the use of sleeve gastrectomy and gastric bypass in the U.S. and compare the complication rates of these bariatric operations.
Background: Sleeve gastrectomy is an increasingly popular alternative to gastric bypass due to its relative simplicity and evolving data supporting its efficacy. Unfortunately, measurement of complication rates for these procedures may be under-reported because of patients' tendency to seek care across multiple institutions. Comprehensive longitudinal data regarding postoperative complications are necessary to help guide patients and surgeons during bariatric procedure selection.
Methods: Using the Truven Heath Analytics MarketScan® database, which captures all inpatient and outpatient billing clams for individuals and dependents covered by participating employee-sponsored health insurance plans, patients undergoing sleeve gastrectomy or gastric bypass between 2010 and 2015, with at least 180 days of insurance coverage prior to surgery, were identified. Inverse-probability of treatment weighted (IPTW) Kaplan-Meier curves were used to determine standardized incidences of postoperative complications and IPTW Cox proportional hazards regression was used to compare rates across procedures. IPTWs were estimated using logistic regression, adjusting for patient sex, age, comorbidities, inpatient procedure status, and procedure year.
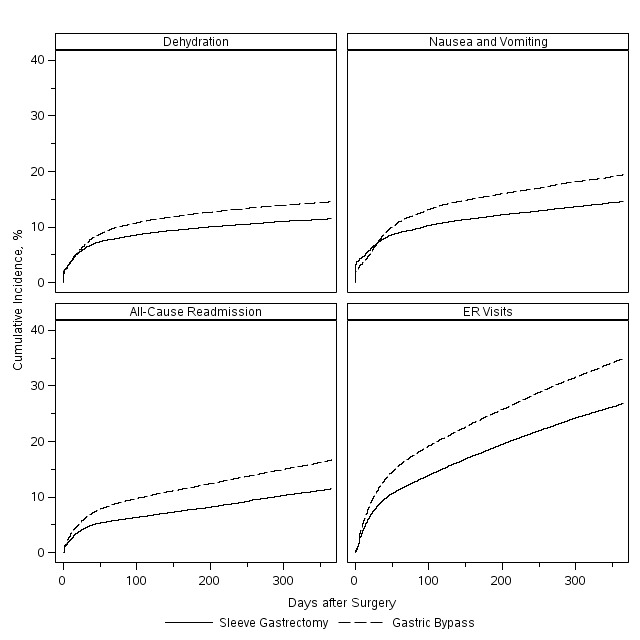
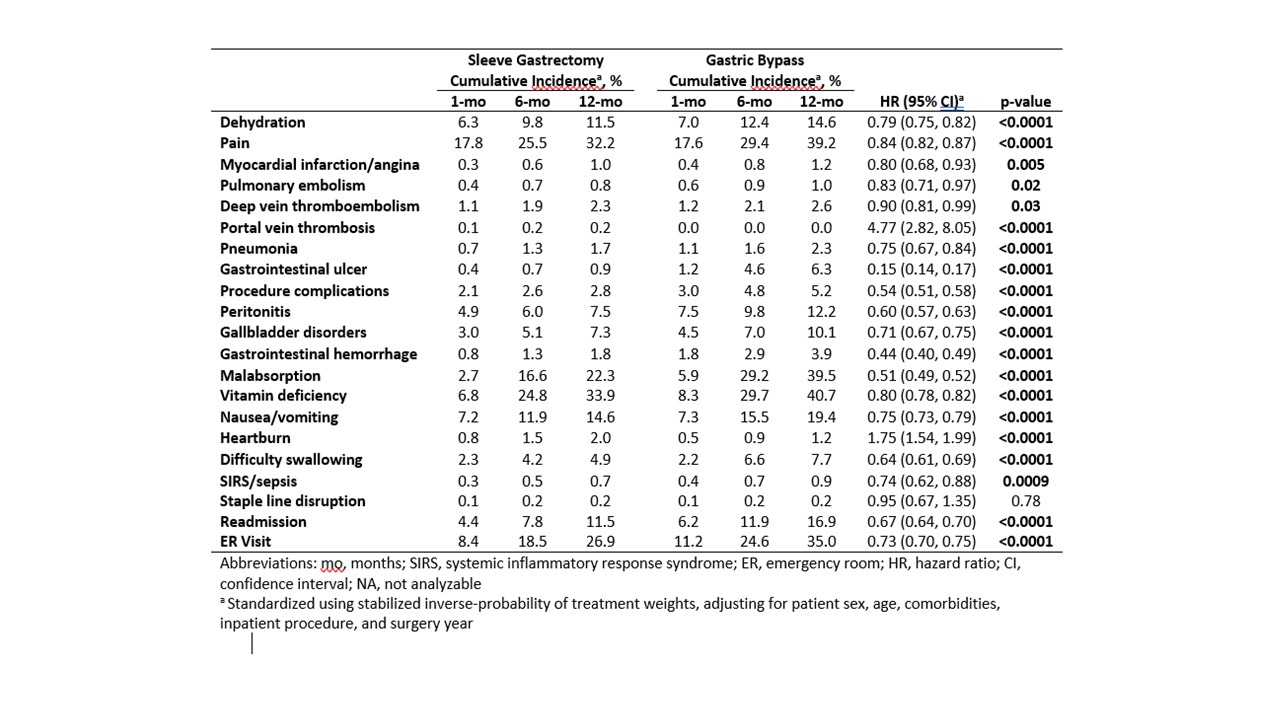
Results: Of the 129,574 patients meeting search criteria, 73,490 (57%) had sleeve gastrectomy and 56,084 (43%) had gastric bypass. The use of sleeve gastrectomy significantly increased from 9% of all bariatric procedures in 2010 to 71% in 2015 (p<0.0001). Median follow-up was 423 days (IQR 165-835). Sleeve gastrectomy patients were less likely to have inpatient surgery (73% vs. 89%, p<0.0001) and diabetes (29% vs. 40%, p<0.0001). After standardization, patients undergoing sleeve gastrectomy were overall less likely to have postoperative complications (Table 1). Notably, sleeve gastrectomy patients had lower incidences of postoperative nausea and vomiting (hazard ratio [HR] 0.75, 95%CI 0.73, 0.79), dehydration (HR 0.79, 95%CI 0.75, 0.82), readmission for any reason (HR 0.67, 95%CI 0.64, 0.70), and emergency room visits (HR 0.73, 95%CI 0.70, 0.75) (Figure 1). Gastric sleeves had higher rates of postoperative heartburn (HR 1.75, 95% CI1.54, 1.99) and portal vein thrombosis (HR 4.77, 95%CI 2.82, 8.05). No difference was seen in staple line leak rates (HR 0.95, 95%CI 0.67, 1.35).
Conclusion: Vertical sleeve gastrectomy has surpassed gastric bypass in utilization across the U.S. It is reassuring that overall postoperative complication rates are lower relative to gastric bypass with the exception of heartburn and portal vein thrombosis.
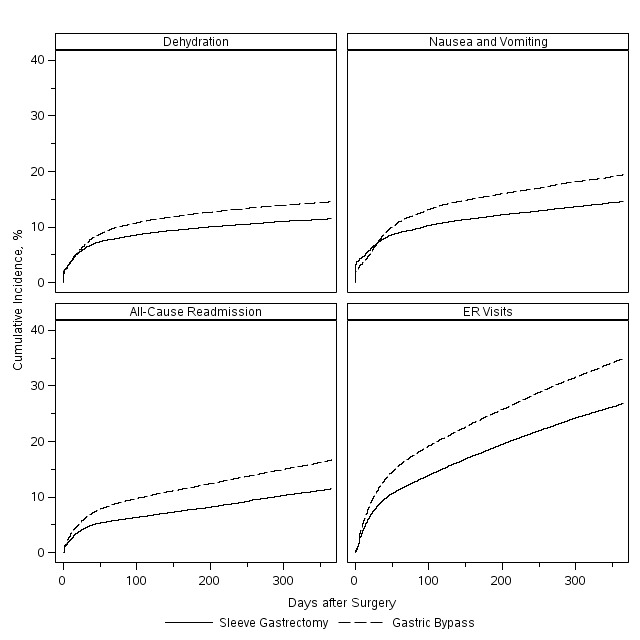
Figure 1. Cumulative incidence of representative complications after sleeve gastrectomy and gastric bypass over 1 year.
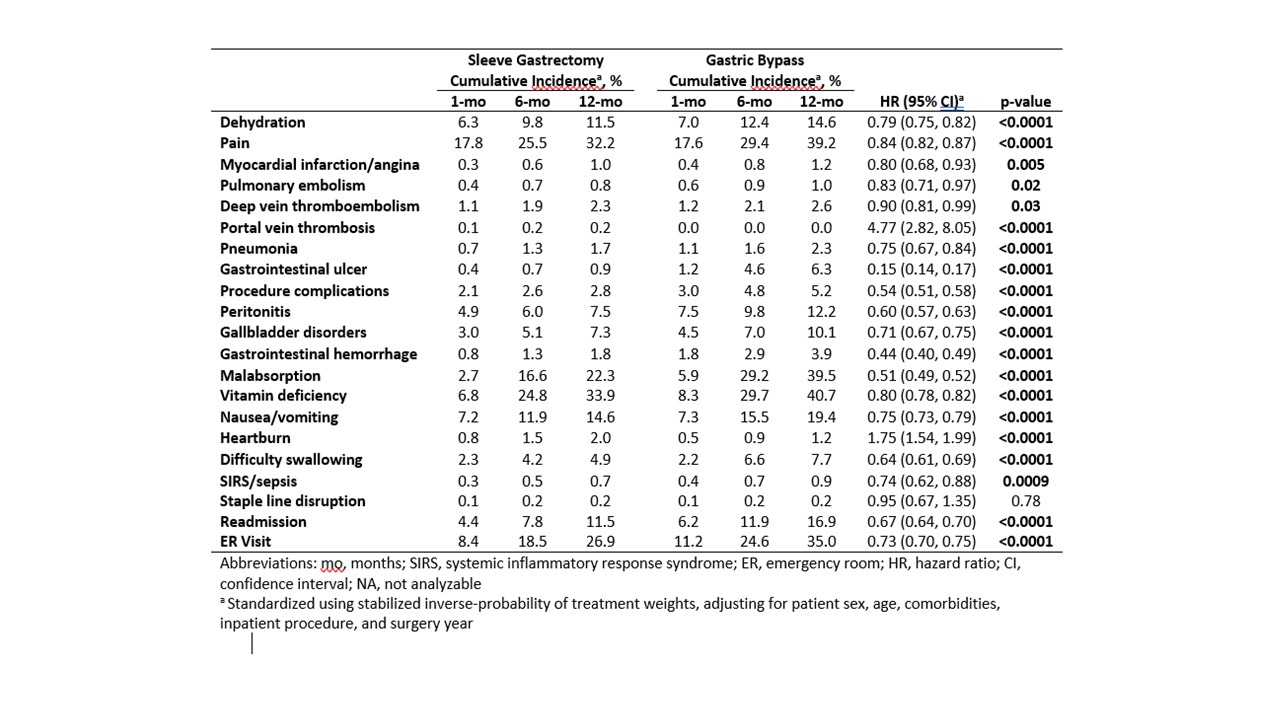
Table 1. Standardized incidence of representative complications after gastric sleeve, compared to gastric bypass.
Back to 2018 Program and Abstracts
|