|
Back to 2018 Program and Abstracts
SURGICAL MANAGEMENT OF GASTROESOPHAGEAL REFLUX DISEASE IN PATIENTS WITH SEVERE ESOPHAGEAL DYSMOTILITY: A PROSPECTIVELY COLLECTED CLINICAL DATA BASE REVIEW
Priscila R. Armijo*1, Akshay Chauhan2, Austin Wheeler1, Dmitry Oleynikov1
1University of Nebraska Medical Center, Omaha, NE; 2University of Colorado, Aurora, CO
Background
Patients with gastroesophageal reflux disease (GERD) and esophageal dysmotility disorders are often told they are not candidates for fundoplication due to fears of worsening dysphagia. However, we hypothesized that a tailored partial fundoplication may improve symptoms in GERD patients who have severe esophageal motility disorders. Our aim was to evaluate the effectiveness of tailored partial fundoplication in the improvement of GERD in non-achalasia esophageal dysmotility patients.
Methods
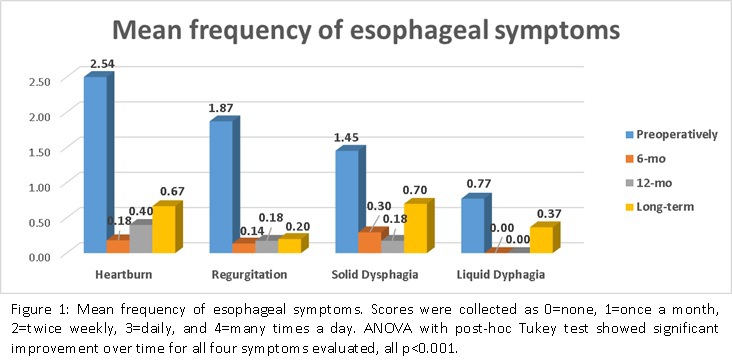
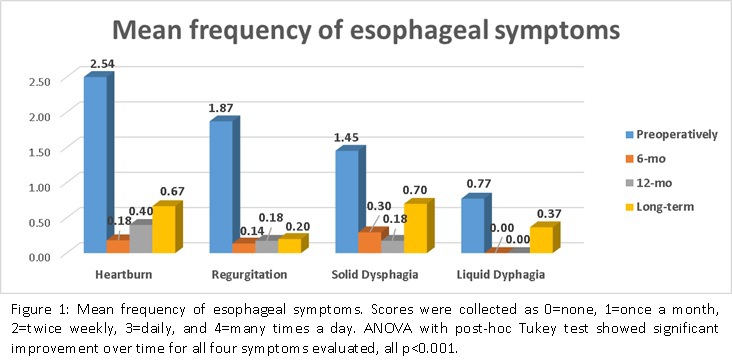
A single-institution prospective database was reviewed for patients with GERD and previous diagnosis of non-achalasia esophageal motility disorder, who underwent a tailored partial fundoplication between 2007-2016. Inclusion criteria were based on Chicago Classification for amotility of the esophageal body or ineffective esophageal motility. Patients with previous diagnosis of achalasia or diffused esophageal spasm were excluded. Motility studies, pre and post upper gastrointestinal imaging (UGI), esophageal symptom scores, antacid and proton pump inhibitor use were all collected. Data were collected pre-operatively (pre-op), at 6-month (6-mo), 12-month (12-mo) and long-term (LT) follow-up. Statistical analysis was made using SPSS v.23.0.0 using ANOVA with post-hoc Tukey tests, with α=0.05.
Results
Among the 548 patients diagnosed with GERD, 54 (180Deg: N=2, 270Deg: N=52) met the inclusion criteria and were included in the study. Eleven (20.4%) patients had amotility of the esophageal body, whereas 79.6% had ineffective peristalsis. Thirty-four (62.9%) were women, mean age was 63±15.1 years, and all underwent laparoscopic tailored partial fundoplication. Mean percentage of peristalsis was 45.3±32.6%, and failed peristalsis was 36.0±32.2%. Mean LES residual pressure was 15.0±18.0mmHg, and 40.7% of patients had hypotensive LES. Mean follow-up time was 25 months [1-7 years]. There was a significant improvement in esophageal symptoms at 6-mo, 12-mo and LT follow-up, compared to pre-op (Figure 1). In addition, there was a significant reduction in use of antacids and proton pump inhibitors after the surgery (pre-op vs 6-mo, pre-op vs 12-mo and pre-op vs LT), all p<0.001. Forty patients (74%) had UGI studies at 12-mo, and all showed persistent dysmotility. Radiographic hiatal hernia recurrence was seen in six patients (11.1%), with only one showing clinical reflux. Three patients required postoperative EGD dilation due to persistent dysphagia.
Conclusion
This study demonstrates the efficacy of tailored partial fundoplication in symptom relief including dysphagia for non-achalasia patients with severe esophageal motility disorders and GERD. Significant symptom improvement, low rate of hiatal hernia recurrence and freedom from PPI clearly indicates that a tailored partial fundoplication is effective in patients with esophageal dysmotility and GERD.
Back to 2018 Program and Abstracts
|