|
 |
Back to 2018 Program and Abstracts
REGIONAL DIFFERENCES IN THE UTILIZATION OF PALLIATIVE CARE IN GERIATRIC COLORECTAL CANCER PATIENTS REQUIRING EMERGENT SURGERY
Danielle R. Heller*1, Raymond A. Jean1,2, Alexander S. Chiu1, Shelli I. Feder3, Vadim Kurbatov1, Charles Cha4, Sajid A. Khan4
1Department of Surgery, Yale School of Medicine, New Haven, CT; 2Department of Medicine, National Clinician Scholars Program, Yale School of Medicine, New Haven, CT; 3US Department of Veteran Affairs, West Haven, CT; 4Department of Surgery, Section of Surgical Oncology, Yale School of Medicine, New Haven, CT
Background:
The benefits of palliative care (PC) for patients with critical illness have been validated across a range of diseases, yet it remains underutilized in surgical patients for unclear reasons. The purpose of this study is to analyze patient and hospital factors predictive of PC utilization for elderly patients with colorectal cancer (CRC) undergoing emergent intestinal surgery.
Methods:
The National Inpatient Sample was queried for patients aged ≥65 years urgently admitted through the emergency department with a diagnosis of CRC from 2009 to 2014. Patients who underwent colectomy, enterectomy or ostomy formation were included and stratified according to documentation of PC consultation during admission. Chi-squared test identified unadjusted differences between groups, and multivariable logistic regression identified predictors of PC.
Results:
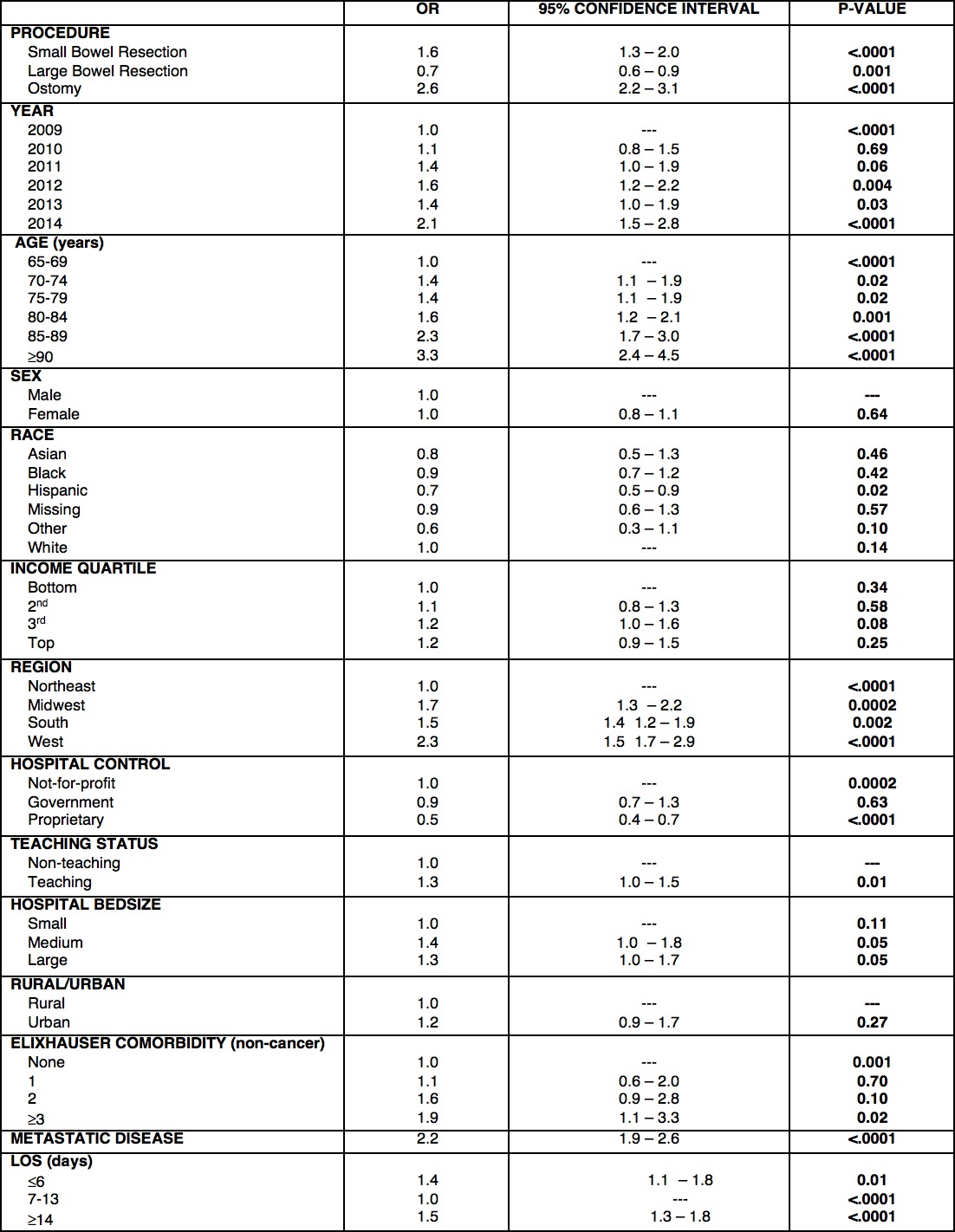
A total of 86,573 discharges met inclusion criteria, of which only 3598 (4.2%) had a PC consultation during admission. Large bowel resection (86.6%) and/or ostomy formation (30.4%) accounted for the majority of cases. The frequency of PC consults increased over time (2.9% in 2009 to 6.2% in 2014, P<0.0001). PC consults were almost twice as likely to occur in the West compared to the Northeast (5.7% vs 3.3%, P<0.0001) and in urban compared to rural settings (4.3% vs 2.8%, P=0.01). PC patients were more likely to present with metastases (60.1% vs 39.9%, P<0.0001) and die prior to discharge (41.5% vs 6.4%, P<0.0001). On multivariable logistic regression, positive predictors of PC utilization (P<0.05) were hospital region outside the Northeast, teaching hospital status, metastatic disease, LOS<7 days, LOS 14+ days, increasing age, and 3 or more comorbidities.[Table 1]
Conclusions:
In the United States, use of palliative care in geriatric patients requiring emergent surgery for CRC is low. The exact reasons for this underutilization are unclear, however, regional variation as well as urban settings appear to play important roles. With increasing evidence suggesting that PC improves cancer patients' quality of life and outcome, understanding the factors and barriers associated with PC consultation for our surgical cancer patients is paramount.
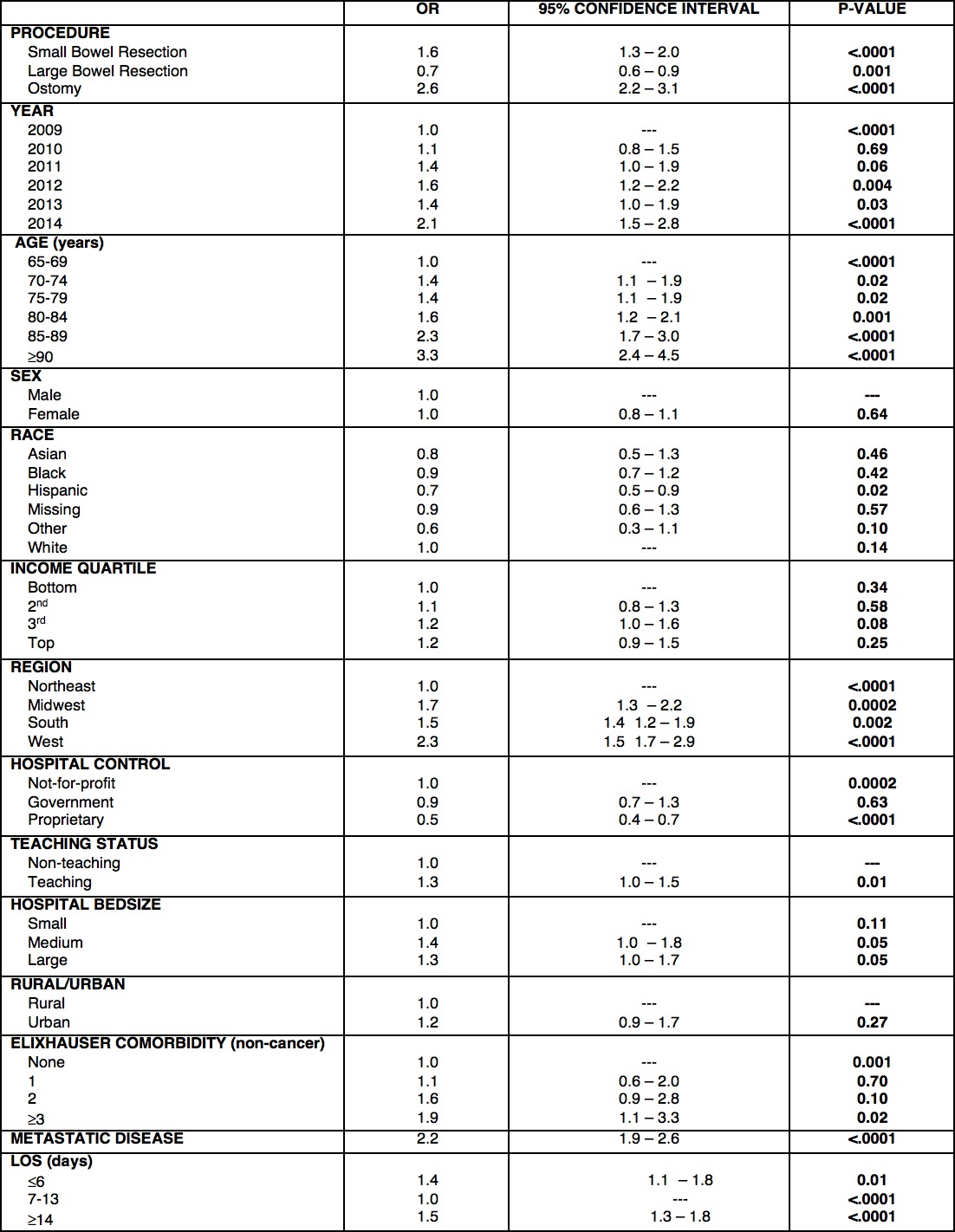
Table 1. Multivariable logistic regression showing strength of association between palliative care consultation and demographic, clinical, and hospital factors.
Back to 2018 Program and Abstracts
|