|
Back to 2018 Program and Abstracts
ONCOLOGICAL OUTCOMES OF PATIENTS WITH LOCALLY ADVANCED RECTAL CANCERS AND LATERAL PELVIC LYMPH NODE INVOLVEMENT
Ipek Sapci*1, Conor P. Delaney1, David Liska1, Sudha Amarnath2, Matthew Kalady1, Scott Steele1, Emre Gorgun1
1Colorectal Surgery, Cleveland Clinic Foundation, Cleveland, OH; 2Radiation Oncology, Cleveland Clinic, Cleveland, OH
Introduction
Optimal management of lateral pelvic nodal disease in locally advanced rectal cancer remains debatable. Lateral pelvic node dissection is currently not considered as part of the routine treatment algorithm in patients with lateral pelvic nodal disease. The aim of our study is to compare local recurrence rates and oncological outcomes of patients with locally advanced rectal cancer between patients with and without lateral pelvic nodal disease involvement.
Methods
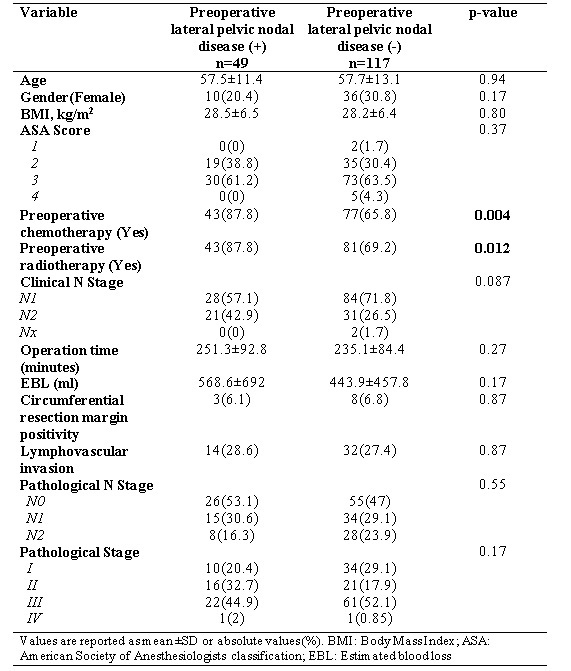
Patients who underwent curative surgery for Stage III rectal adenocarcinoma between 2009-2014 and had a preoperative MRI were included in our study. Patients with positive lateral pelvic nodal disease (iliac or obturator nodes) on preoperative MRI were compared to patients with no lateral pelvic nodal disease (LPND). Patients without a preoperative MRI and patients with recurrent rectal cancer were excluded. Data were collected from a prospectively maintained institutional database and additional chart reviews were conducted as needed. Univariate analysis was done to compare differences between the groups including demographics, perioperative variables and pathological outcomes. Log-rank test was used to evaluate overall and disease-free survival between the groups.
Results
A total of 166 patients were included in our study with a mean age of 57.6±12.6 and 72% were male. Demographics, perioperative variables and pathological outcomes are listed in the Table. 49/166 (29.5%) of the patients had positive LPND on preoperative MRI. 17 out of 49 patients had a post-neoadjuvant treatment MRI and 15 patients had a decrease in size of nodes or disappearance of LPND. On univariate analysis, groups were comparable with respect to demographics and preoperative comorbidities. Median follow-up was 44 months (CI: 41.0, 50.0). Local recurrence rates of patients with LPND were higher, however this did not reach statistical significance (61.5% vs. 32%, p=0.09). Overall and disease-free survival were comparable between the groups on Log-rank test (p=0.46, p=0.73).
Conclusions
Overall and disease-free survival rates are similar in patients with locally advanced rectal cancer with or without positive LPND. Higher local recurrence rates in patients with LPND may warrant further studies to determine the role of routine lateral pelvic lymph node dissection.
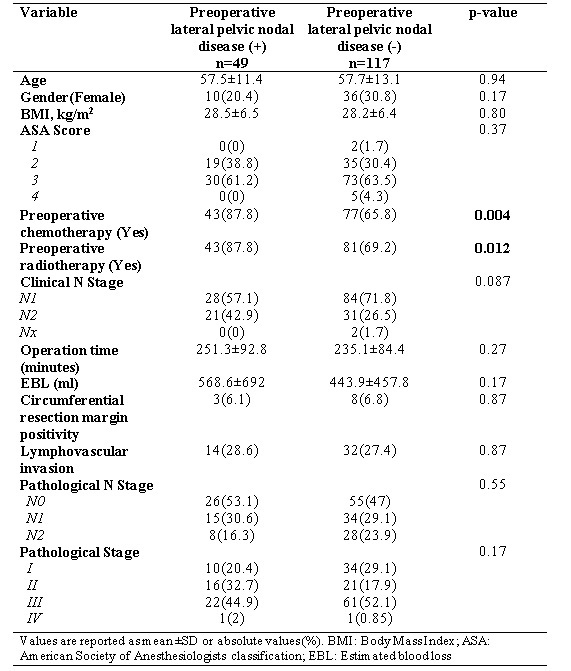
Table. Univariate analysis results of comparison between two groups in terms of demographics, peri-operative and pathologic variables.
Back to 2018 Program and Abstracts
|