|
 |
Back to 2018 Program and Abstracts
SURGEON-LEVEL VARIATION IN UTILIZATION OF NEOADJUVANT THERAPY FOR LOCALLY ADVANCED RECTAL ADENOCARCINOMA
Douglas S. Swords*2,1, David E. Skarda2,1, William T. Sause3, Ute Gawlick2, George M. Cannon3, Mark A. Lewis3, Jesse Gygi3, H T. Kim2
1Surgery, University of Utah, Salt Lake City, UT; 2Surgical Services Clinical Program, Intermountain Healthcare, Salt Lake City, UT; 3Oncology Services Clinical Program, Intermountain Healthcare, Salt Lake City, UT
Background: Neoadjuvant therapy for clinical stage II-III rectal adenocarcinoma has been standard of care for over a decade, and delivery of preoperative chemoradiation to such patients is a Commission on Cancer quality metric. National Cancer Database studies have shown that only 75% of appropriate patients receive neoadjuvant therapy, but the determinants of this failure to deliver evidence-based therapy remain largely unknown. We aimed to determine the underlying reasons for omission of neoadjuvant therapy using granular clinical data from a 22-hospital system.
Methods: This is a retrospective study of patients with clinical or pathologic stage II-III rectal adenocarcinoma treated with initial curative intent from 2010-2016 in an Intermountain Healthcare hospital. Patients who were stage I by endoscopic ultrasound or MRI who were upstaged to pathologic stage II-III at surgery were excluded (N=12). Covariates with a univariate P<0.2 were included in a multivariable logistic regression model for predictors of omission of neoadjuvant therapy. Risk ratios and adjusted risk differences were obtained using marginal standardization. Risk- and reliability-adjusted rates of neoadjuvant therapy were calculated for surgeons who treated ≥3 patients. Rates of positive margins (positive proximal/distal margin or circumferential radial margin ≤ 1 mm) and long-term outcomes were examined after excluding patients who were not resected(N=4) or who underwent local excision(N=6).
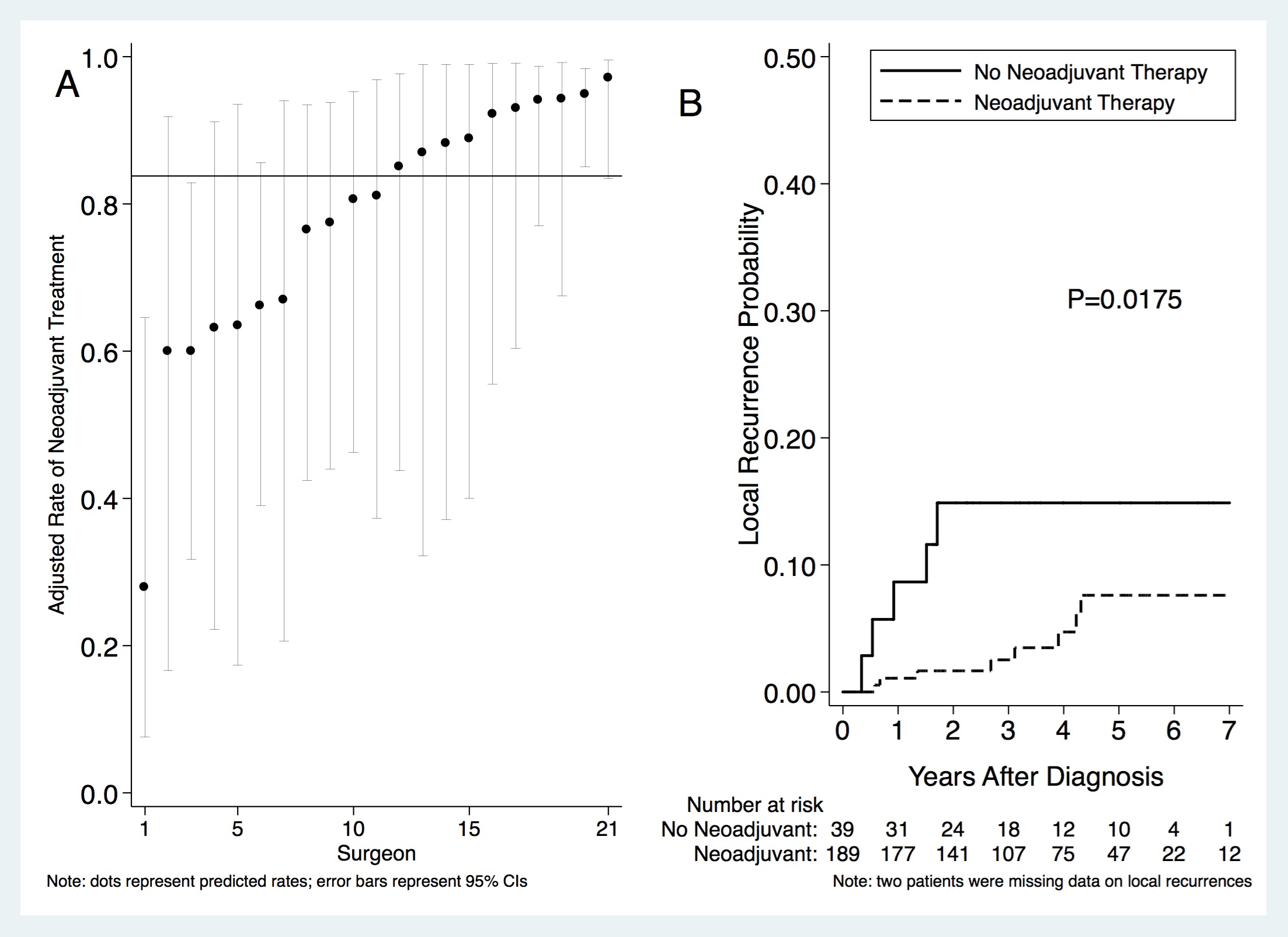
Results: There were 240 patients with clinical stage II-III or undocumented clinical stage/pathologic stage II-III rectal cancer who were treated by 36 surgeons at 9 hospitals. Three surgeons treated 122/240 patients (50.8%). Neoadjuvant therapy was omitted in 41/240 (17.1%). Processes of care in which neoadjuvant therapy was omitted and independent predictors of omission of neoadjuvant therapy are shown in the Table. Among 21 surgeons who treated ≥ 3 cases, adjusted rates of neoadjuvant therapy varied 3.5-fold (28% to 97%, Figure A). Rates of positive margins were higher in patients who did not receive neoadjuvant therapy: 8/40 (20.0%) vs. 16/190 (8.4%) (P=0.03, chi-square). Neoadjuvant therapy was associated with lower rates of local recurrences (P=0.0175, log-rank, Figure B) but no differences in rates of distant metastases, disease-specific survival, or overall survival (P>0.26 for all, log-rank, not shown).
Conclusions: The dominant risk factors for omission of neoadjuvant therapy are tumor location in the upper rectum and treatment by a low volume surgeon. Surgeon rates of neoadjuvant therapy varied 3.5-fold, and low volume surgeons utilized neoadjuvant therapy less often. Neoadjuvant therapy was associated with lower rates of positive margins and local recurrences. Initiatives that give low-utilizing surgeons feedback about appropriate utilization of neoadjuvant therapy are warranted.
Processes of Care and Factors Associated with Omission of Neoadjuvant Therapy
| Processes of Care in Patients Where Neoadjuvant Therapy was Omitted (N=41) | | Process of Care | N (%) | | Taken directly to surgery without EUS or MRI | 19(46.3%) | | Thought to be sigmoid cancer preoperatively | 11 (26.8%) | | "Urgent" presentation (obstruction, substantial bleeding, or perforation) | 4 (9.8%) | | Upfront surgery even though cT3-T4 and/or cN1 on EUS or MRI | 3 (7.3%) | | Concerns about functional status | 2 (4.9%) | | Synchronous colon cancer | 1 (2.4%) | | Tumor not thought to be an invasive cancer preoperatively | 1 (2.4%) | | Multivariable Analysis of Factors Associated with Omission of Neoadjuvant Therapy | | | Risk Ratio
(95% CI) | Adjusted Absolute Risk Difference
(95% CI) | P | | Female sex (vs. male) | 1.78 (1.11, 2.87) | 9.4 (3.1, 15.7) | 0.003 | | Cancer history (vs. none) | 2.31 (1.26, 4.22) | 19.9 (1.7, 38.1) | 0.03 | | Location (vs. ≤ 6 cm from anal verge) | | | | | 6.01-12 cm | 1.70 (0.75, 3.86) | 6.7 (-4.9, 18.3 | 0.26 | | > 12 cm | 4.35 (2.67, 7.09) | 32.1 (20.8, 43.3) | <0.001 | | Urgent presentation | 1.86 (0.90, 3.84) | 13.9 (-8.6, 36.4) | 0.22 | | Colorectal surgeon | 0.91 (0.49, 1.66) | -1.6 (-11.6, 8.3) | 0.75 | | Surgeon volume (vs. > 3 cases/year) | | | | | ≤ 3 cases/year | 9.45 (2.78, 32.06) | 25.1 (14.0, 36.2) | <0.001 |
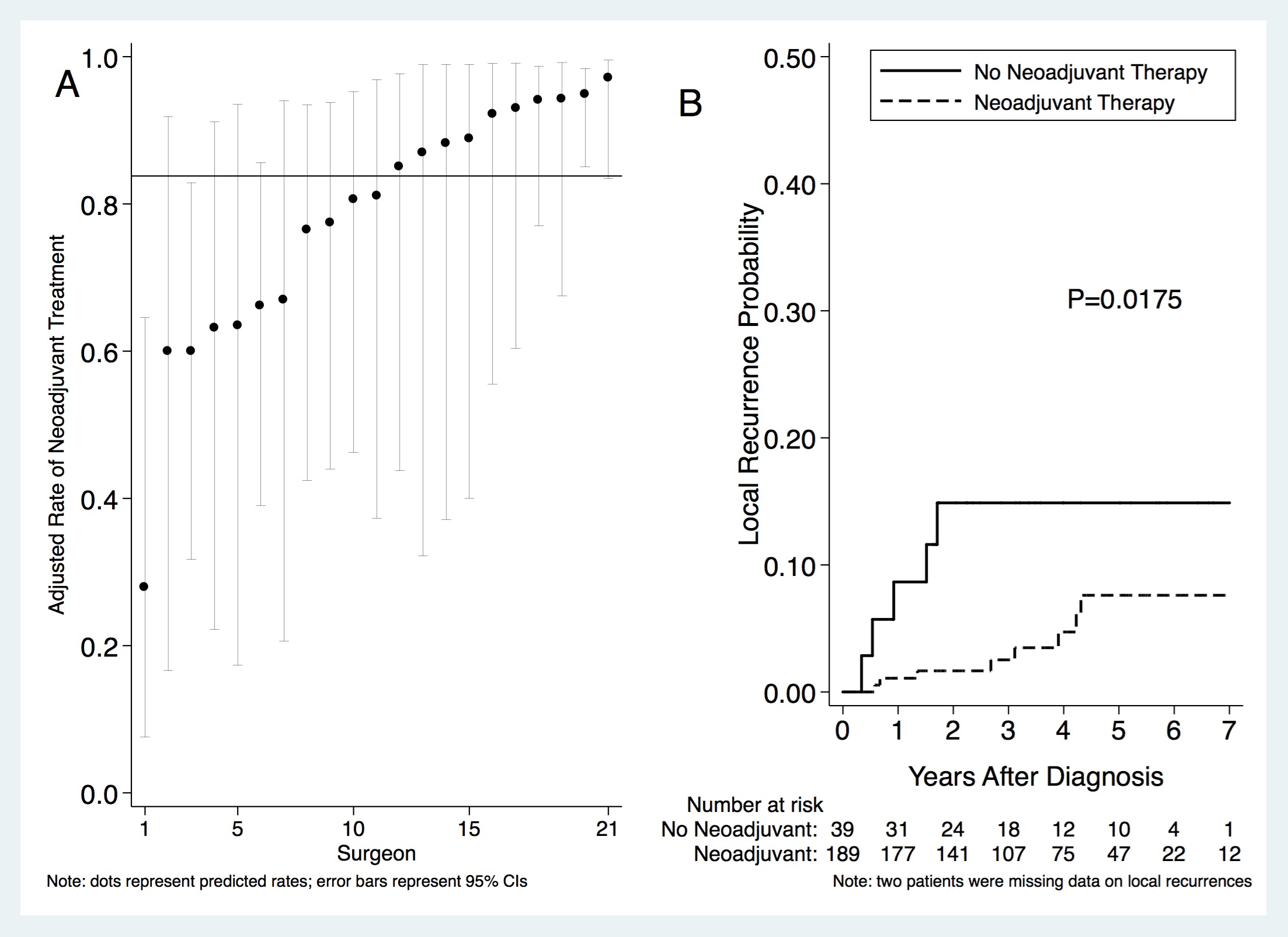 Risk- and reliability adjusted rates of neoadjuvant therapy among surgeons that treated ≥ 3 patients (A) and cummulative probability of local recurrences (B)
Back to 2018 Program and Abstracts
|