|
 |
Back to 2018 Program and Abstracts
THE DILEMMA OF THE DILATED MAIN PANCREATIC DUCT IN THE DISTAL PANCREATIC REMNANT AFTER PROXIMAL PANCREATECTOMY FOR INTRADUCTAL PAPILLARY MUCINOUS NEOPLASM
Rachel E. Simpson*1, Eugene P. Ceppa1, Howard Wu2, Fatih Akisik3, Michael G. House1, Nicholas J. Zyromski1, Attila Nakeeb1, Mohammad A. Al-Haddad4, John DeWitt4, Stuart Sherman4, C. Max Schmidt1
1Surgery, Indiana University, Indianapolis, IN; 2Pathology, Indiana University, Indianapolis, IN; 3Radiology, Indiana University, Indianapolis, IN; 4Gastroenterology, Indiana University, Indianapolis, IN
OBJECTIVE(S): The presence of a dilated main pancreatic duct (MPD) in the distal pancreatic remnant (DPR) after proximal pancreatectomy (PP) for intraductal papillary mucinous neoplasm (IPMN) has become an increasingly recognized diagnostic dilemma. We sought to determine parameters predictive of main duct IPMN (MD-IPMN) and malignancy during surveillance.
METHODS: A retrospective review of a prospectively maintained database revealed 317 patients who underwent PP for IPMN (1992-2016) at a university hospital. MPD dilation was defined as >5mm or "dilated" on radiographic reports. Strong suspicion for MD-IPMN was based on the physician's overall impression from preoperative studies. Statistics compared groups using the students T test for continuous variables, and the Chi Square or Fisher's Exact test for categorical variables with P < 0.05 considered significant.
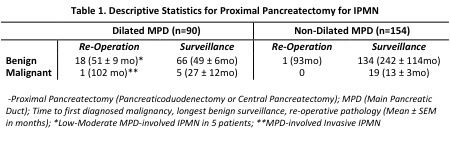
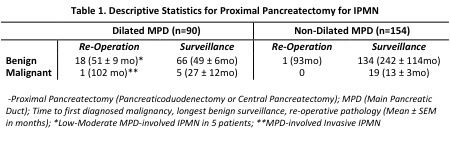
RESULTS: Outcomes of 244 patients who underwent primary surveillance follow-up at our institution are in Table 1. Invasive IPMN or adenocarcinoma on surgical pathology at the time of PP was the only significant predictor of a subsequent malignant outcome (95.8% of malignant outcomes P <0.001) in surveillance follow-up. Low/Moderate grade lesions had a non-malignant surveillance outcome at last follow-up regardless of duct diameter or any other factors considered. Nineteen of 20 (95%) patients who underwent DPR surgery had a dilated MPD in the DPR. Six (32%) had MD-IPMN on DPR resection pathology. Patients with MD-IPMN on DPR resection pathology had greater MPD dilation both at the time of PP (7.3 vs 5.8mm, P=0.55) and DPR resection (8.9 vs 6.4mm, P=0.078), but this was not statistically significant. Parameters with greatest sensitivity (>70%) to predict MD-IPMN in the DPR were high quantity DNA and mucin in MPD fluid analysis [via endoscopic ultrasound (EUS) fine needle aspiration (FNA)], MPD dilation in the DPR, absence of pancreaticojejunal anastomotic stenosis on EUS-directed ductogram, exocrine insufficiency and the surgeon's strong suspicion. Factors with the greatest specificity were high quality DNA, KRAS mutation, GNAS mutations, or LOH mutations in EUS-FNA derived MPD fluid analysis, cytology with high grade atypia, a positive margin for IPMN at PP, unintentional weight loss and the endoscopist's strong suspicion.
CONCLUSIONS: MPD dilation in the DPR after PP for IPMN remains a diagnostic dilemma. Several parameters show promise in the accurate diagnosis of MD-IPMN in the DPR.
Back to 2018 Program and Abstracts
|