|
 |
Back to 2018 Program and Abstracts
CHROMOGRANIN A AND PREDICTING RECURRENCE IN PANCREATIC NEUROENDOCRINE TUMORS: A NOVEL PRE-OPERATIVE RISK SCORING SYSTEM
Alexander Fisher*1, Alexandra G. Lopez-Aguiar8, Victoria Rendell1, Courtney Pokrzywa1, Flavio G. Rocha7, Zaheer Kanji7, George A. Poultsides3, Eleftherios A. Makris3, Mary Dillhoff6, Eliza W. Beal6, Ryan Fields2, Panni Roheena2, Kamran Idrees5, Paula Marincola Smith5, Clifford S. Cho4, Megan V. Beems1, Shishir K. Maithel8, Emily R. Winslow1, Daniel E. Abbott1, Sharon M. Weber1
1Department of Surgery, University of Wisconsin, Madison, WI; 2Washington University in St. Louis, St. Louis, MO; 3Stanford University, Stanford, CA; 4University of Michigan, Ann Arbor, MI; 5Vanderbilt University, Nashville, TN; 6The Ohio State University Comprehensive Cancer Center, Columbus, OH; 7Virginia Mason Medical Center, Seattle, WA; 8Department of Surgery, Emory University, Atlanta, GA
INTRO: Chromogranin A (CgA) may be prognostic for patients with neuroendocrine tumors. However, the value of incorporating CgA level into pre-operative risk stratification has not been evaluated in a large multi-institutional study.
METHODS: Patients undergoing resection for pancreatic neuroendocrine tumors (pNET) were selected from the 8 institutions of the US Neuroendocrine Tumor Study Group database. Of 296 patients, a stratified random sample of 232 (78% of cohort) was used for risk score development, with the remaining 64 (22%) used for risk score validation. Patients were grouped by CgA level in reference to the upper limit of normal (ULN) as follows: normal, 1-5x ULN, and >5x ULN. Cox regression was used to identify pre-operative variables that predicted recurrence-free survival (RFS), and those with p<0.1 were included in a risk score. Logistic regression was used to evaluate the risk score for predicting tumor recurrence in the validation cohort.
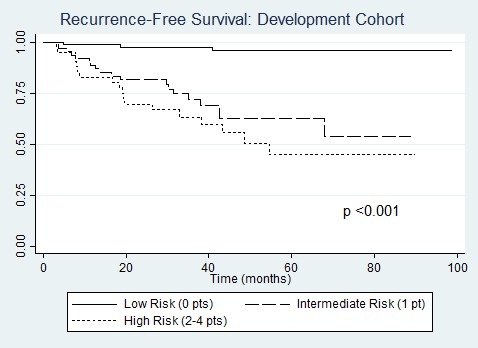
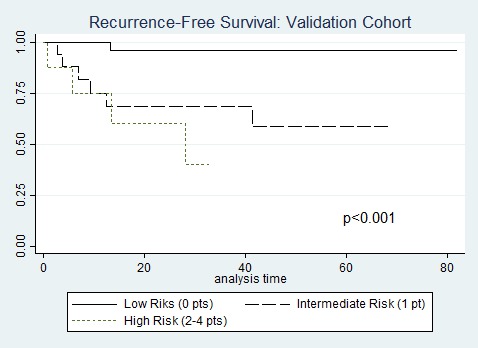
RESULTS: In the entire cohort, 251 (85%) patients had localized pancreatic tumors, 27 (9%) synchronous metastases, and 18 (6%) underwent resection for recurrent pNETs. All patients were treated with curative intent resection of all disease sites. Grade 2 or 3 tumors were present in 79 patients (34%), 86 (29%) had primary tumor size ≥ 4 cm. Median follow-up time was 37 months, and 5-year RFS was 75% [95% CI 68%-81%]. Those with CgA >5x ULN (n=28) had 5-year RFS of 63%, compared to 75% for 1-5x ULN (n=88), and 77% for normal (n=180, p=0.15). Cox regression analysis in the risk score development cohort yielded four variables meeting criteria for inclusion in the risk score: CgA >5x ULN (HR 4.4, p=0.01), tumor grade 2/3 (HR 3.9, p=0.01), resection for recurrent disease (HR 5.9, p<0.01), and tumor size >4 cm (HR 4.5, p=0.1). These four variables were assigned 1 point each in the risk score model given significant overlap of 95% CI for HR estimates. Patient stratification into low risk (0 points, n=111, 48%), intermediate risk (1 point, n=73, 31%), and high risk (≥2 points, n=48, 21%) groups resulted in significant survival discrimination between groups in both the development cohort (5-yr RFS for low risk 96%, intermediate 63%, and high risk 45%, p<0.001; Figure) and validation cohort (5-yr RFS for low risk 96%, intermediate 59% and high risk 0%, p<0.001; Figure). Risk-score testing in the unique validation cohort of 64 patients resulted in an area under ROC curve of 0.78 with 92% specificity, 33% sensitivity, NPV of 86%, and PPV of 50%.
DISCUSSION: A simple pre-operative risk scoring system that incorporates CgA level, tumor grade, tumor size, and presence of recurrent tumors resulted in a high degree of specificity for identifying patients at low-risk for tumor recurrence. This test can be utilized preoperatively to aid informed decision making.
Recurrence-free survival by risk score in the risk score development cohort.
Recurrence-free survival by risk score in the risk score validation cohort.
Back to 2018 Program and Abstracts
|