|
 |
Back to 2018 Program and Abstracts
EVOLVING THE PARADIGM OF EARLY DRAIN REMOVAL FOLLOWING PANCREATODUODENECTOMY
Thomas Seykora*1, Laura Maggino1,2, Giuseppe Malleo2, Major Kenneth Lee1, Robert E. Roses1, Claudio Bassi2, Charles Vollmer1
1Surgery, University of Pennsylvania, Philadelphia, PA; 2Surgery, University of Verona, Verona, Italy
Background: Recent data illustrates improved outcomes when adhering to selective and early removal of drains following pancreatoduodenectomy (PD). However, the mechanics underlying this paradigm, including selection of candidates, determinants of outcomes, and consensus of an "early" timeframe, remain nebulous. Given these challenges, this study aims to clarify the dynamic nature of the early drain removal concept.
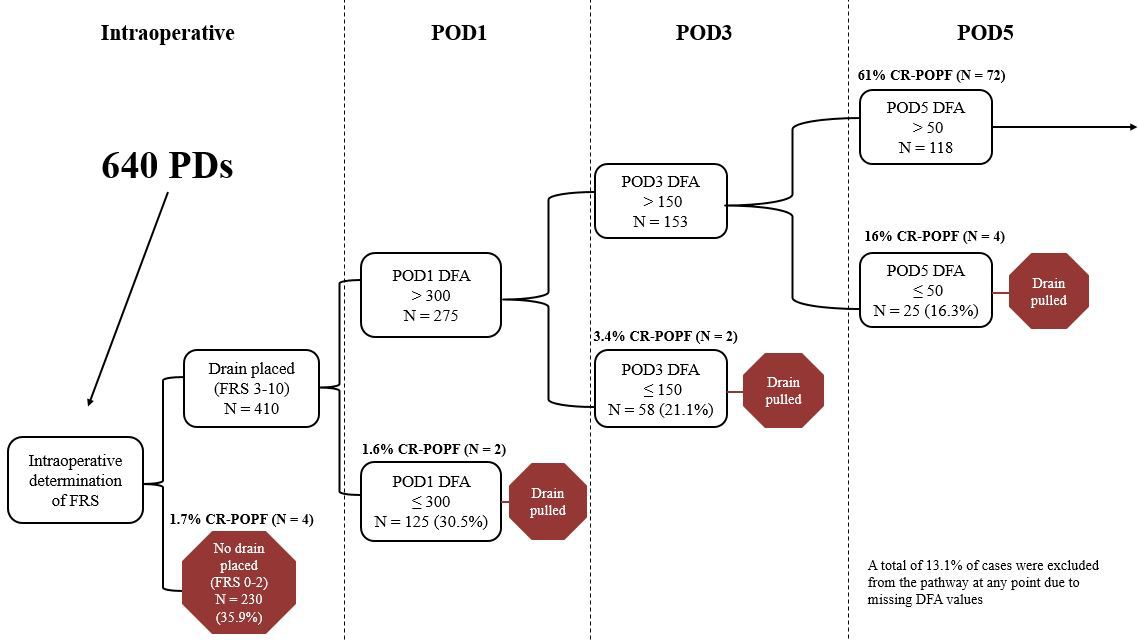
Methods: 640 PDs, performed at two institutions (2014-17), were managed by a general policy of selective drain placement using the fistula risk score (FRS), paired with early removal based on a POD1 drain fluid amylase (DFA) threshold of 5000. Outcomes were reappraised in the framework of a novel proposal whereby intraoperative drain omission was utilized based on a low-risk profile (FRS 0-2), followed by drain removal sequentially at PODs 1, 3, & 5 if DFA fell below specific cutoffs based on optimized negative predictive values (NPV) for CR-POPF. Characteristics and outcomes of the ultimate cohort, enriched for CR-POPF risk, were analyzed using uni- and multivariable analyses (MVA).
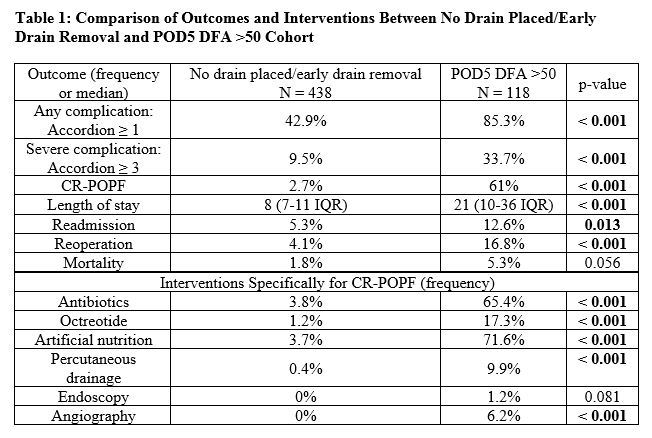
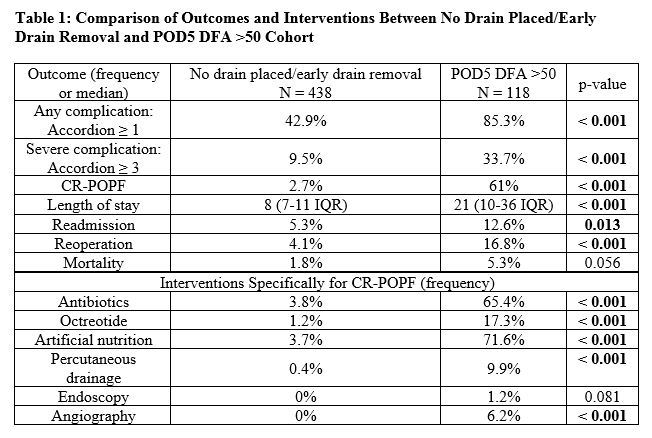
Results: The overall CR-POPF rate was 15.2% (13.3% grade B; 1.9% grade C). Median DFA POD1, 3, & 5 were 440 (IQR 55-2977), 94 (20-518), and 150 (42-609), respectively. Intraoperative FRS calculation would preclude drains from 230 (35.9%) negligible/low risk cases with a resulting cohort CR-POPF rate of 1.7% (Fig 1). Of the remaining 410 patients, 30.5% would have drains removed on POD1 based on a DFA threshold of 300 (NPV=98.4%), demonstrating a 1.6% CR-POPF rate. Next, on POD3, drains could be removed in the residual cohort from 21.1% of patients whose DFA was ≤150 (NPV=96.6%), reflecting a 3.4% CR-POPF rate. Likewise, on POD5, a DFA threshold of 50 (NPV=84%) identified 16.3% more patients whose drains could be removed. The remaining "enriched" cohort (POD5 DFA >50), reflecting just 18.4% of the original patients, displays a 61% CR-POPF rate. This group has markedly worse outcomes compared to those patients with no drain or early drain removal (Table 1), and drains were removed on a median of POD9 (CR-POPF: 22[8-34] vs. no CR-POPF: 6[5-7], p<0.001). On POD5, a DFA >2000 threshold best predicted subsequent CR-POPF (PPV = 89.5%). MVA revealed a positive association between pancreatic cancer/pancreatitis and CR-POPF (OR=3.536, p=0.034). Overall, the ability to predict CR-POPF improved temporally across the sequence of management thresholds: intraoperative FRS (AUC=0.688), POD1 (AUC=0.791, p<0.001), POD3 (AUC=0.841, p<0.001), and POD5 (AUC=0.880, p<0.001).
Conclusion: This data suggests a novel paradigm employing the principles of selective drain placement and early removal, which ultimately consolidates CR-POPF prediction. Furthermore, early drain removal is a fluid concept and can be employed throughout the postoperative time course using conditional thresholds.
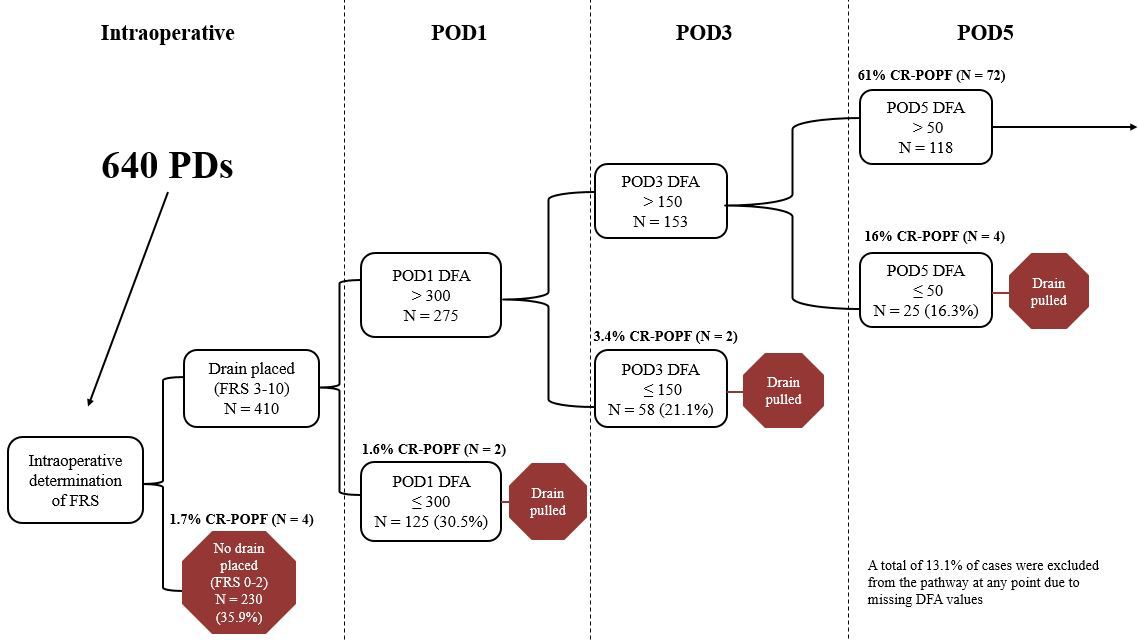
Figure 1: Flow chart depicting proposed drain management pathway with corresponding CR-POPF rates.
Back to 2018 Program and Abstracts
|