|
 |
Back to 2018 Program and Abstracts
OUTCOME OF PATIENTS WITH BORDERLINE RESECTABLE PANCREATIC CANCER IN THE CONTEMPORARY ERA OF NEOADJUVANT CHEMOTHERAPY
Ammar A. Javed*1, Ayat Siddique1, Alex Blair1, Lindsay Parish1, Richard Burkhart1, Matthew J. Weiss1, John Cameron1, Amol Narang2, Lei Zheng3, Daniel Laheru3, Christopher L. Wolfgang1, Jin He1
1Surgery, Johns Hopkins, Baltimore, MD; 2Radiation Oncology, Johns Hopkins, Baltimore, MD; 3Medical Oncology, Johns Hopkins, Baltimore, MD
Introduction
Less than 20% patients presented with resectable pancreatic cancer at diagnosis. After neoadjuvant therapy, some patients with borderline resectable pancreatic cancer (BRPC) may have successful resection with negative margin. The outcome of BRPC patients after neoadjuvant therapy remains unclear.
Methods
A prospectively maintained single-institution database was used to identify patients with BRPC who were managed at the pancreas multidisciplinary clinic between 2013-2016. Data on treatment, course of disease, and outcomes were collected. Outcome measures included rate of resection, response to chemotherapy, and overall survival (OS).
Results
Of 866 patients who presented with pancreatic cancer to our multidisciplinary clinic, 151(17.5%) were staged as BRPC. The remaining patients were staged as having resectable (N=180,20.8%), locally advanced (N=364,42.0%), and metastatic (N=171,19.7%) disease.
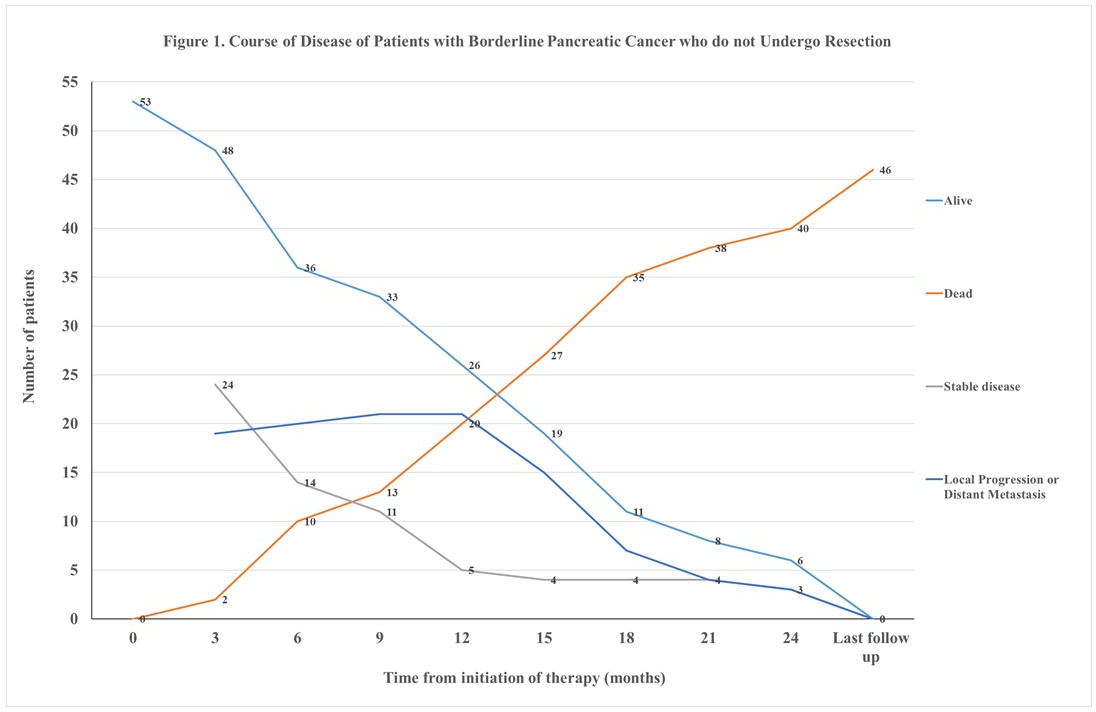
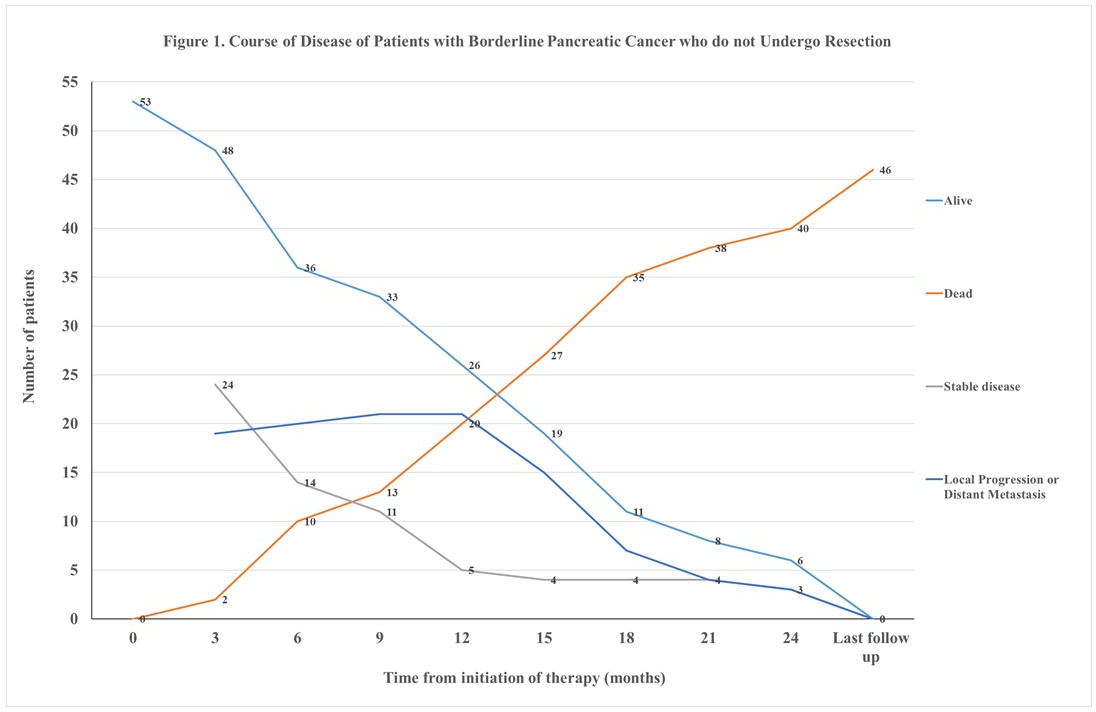
After neoadjuvant therapy, 98(64.9%) patients with BRPC underwent resection. The median survival of resected BRPC patients was 28.6 months compared to 13.2 months of those who did not (p<0.001). The clinical course of 53 BRPC patients who did not undergo resection is summarized in Figure 1. In 10(6.6%) patients surgical resection was attempted but aborted due to progression of local disease or presence of occult metastatic disease. Resection was not attempted in the remaining patients due to radiological evidence of local disease progression (N=14,9.2%) or distant metastasis (N=10,6.6%), intolerance of chemotherapy (N=8,5.3%), or medical comorbidities (N=5,3.3%). At a median follow-up of 11.9 (IQR: 5.3-16.5) months, 47 of 53 BRPC patients had died due to disease progression while 6 (11.3%) were lost to follow-up.
Conclusion
After neoadjuvant therapy, up to one-third of BRPC patients do not undergo resection due to multiple factors. Surgical resection results in a longer survival in patients with BRPC.
Back to 2018 Program and Abstracts
|