|
 |
Back to 2018 Program and Abstracts
SURGERY PROVIDES LONG-TERM SURVIVAL IN PATIENTS WITH METASTATIC NEUROENDOCRINE TUMORS UNDERGOING RESECTION FOR NON-HORMONAL SYMPTOMS
Jeffery Chakedis*1, Eliza W. Beal1, Alexandra G. Lopez-Aguiar6, George A. Poultsides2, Eleftherios A. Makris2, Flavio G. Rocha3, Zaheer Kanji3, Sean Ronnekleiv-Kelly4, Alexander Fisher4, Ryan Fields5, Bradley A. Krasnick5, Kamran Idrees7, Paula Marincola Smith7, Clifford S. Cho8, Megan V. Beems8, Shishir K. Maithel6, Timothy M. Pawlik1, Carl Schmidt1, Mary Dillhoff1
1The Ohio State University, Columbus, OH; 2Stanford University, Palo Alto, CA; 3Virginia Mason Medical Center, Seattle, WA; 4University of Wisconsin School of Medicine and Public Health, Madison, WI; 5Washington University School of Medicine, St. Louis, MO; 6Emory University , Atlanta, GA; 7Vanderbilt University, Nashville, TN; 8University of Michigan, Ann Arbor, MI.
Introduction
Patients with metastatic neuroendocrine tumor (NET) often have an indolent disease course and expected long term survival. Outcomes for patients with metastatic NET undergoing surgery for non-hormonal (NH) symptoms including GI obstruction, bleeding, or pain is not well studied. We evaluated the survival in this population to determine the utility of surgical intervention.
Methods
We identified patients with metastatic gastroenteropancreatic NET who underwent resection from 2000-2016 at 8 academic institutions who participated in the U.S. Neuroendocrine Tumor Study Group. Survival analysis was performed for patients with NH symptoms and logistic regression determined factors predictive of early (1-year) mortality.
Results
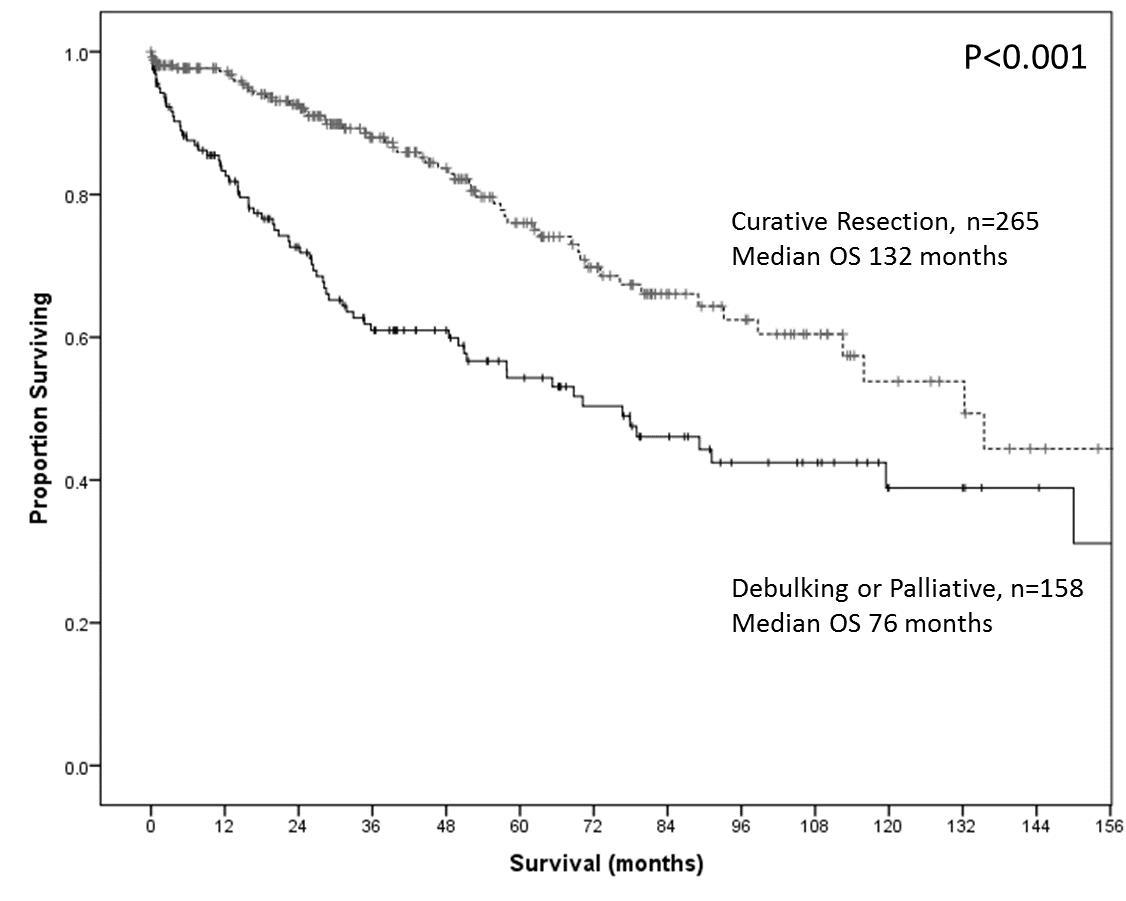
428 patients with metastatic NET to liver 253 (59.1%), lung 10 (2.3%), bone 12 (2.8%), and other sites 129 (30.1%) presented with NH symptoms of pain 300 (70.1%), GI bleeding 55 (12.9 %) GI obstruction 50 (11.7%), and biliary obstruction 38 (8.8%). The median survival was 81.0 months, and was not different based on symptomatology. Operative intent was the strongest predictor of overall survival with 265 patients (62.4%) undergoing curative intent, 114 (26.9%) debulking, and 44 (10.5%) palliative resection. Removal of all metastatic disease was associated with the longest median survival (132.1 months) compared to debulking (79.0 months, OR 2.0, 95%CI 1.3-2.9), or palliative resection (50.0 months, OR 3.4, 2.1-5.6), Figure 1. Of patients undergoing debulking and palliative resection, most were undergoing their first operation 112 (70.0%). 114 (70.3%) had the primary resected with or without metastatic disease, and 45 (28.2%) had resection of symptomatic metastatic disease only. The 3, 6 and 12-month mortality was 14.4%, 18.8%, and 29.4%, respectively. Factors associated with 1-year mortality included operations involving the colon (OR 5.40, 95% CI 1.32-22.18), stomach (14.40, 1.10-189.3), and pancreas (3.60, 1.22-10.59) and was not correlated with the size, differentiation, grade or Ki-67 index of the tumor. The patients who lived past 1 year after debulking or palliative operation had a median survival of 119 months.
Conclusions
Patients with metastatic NET and NH symptoms that necessitate palliative surgery can expect long-term survival albeit less than those who had all disease removed. Factors associated with early mortality after non-curative resection are difficult to predict preoperatively and are associated with tumor locations which require complex procedures. Surgical intervention remains a critical component of multidisciplinary care of patients with metastatic NET, particularly for symptomatic patients.
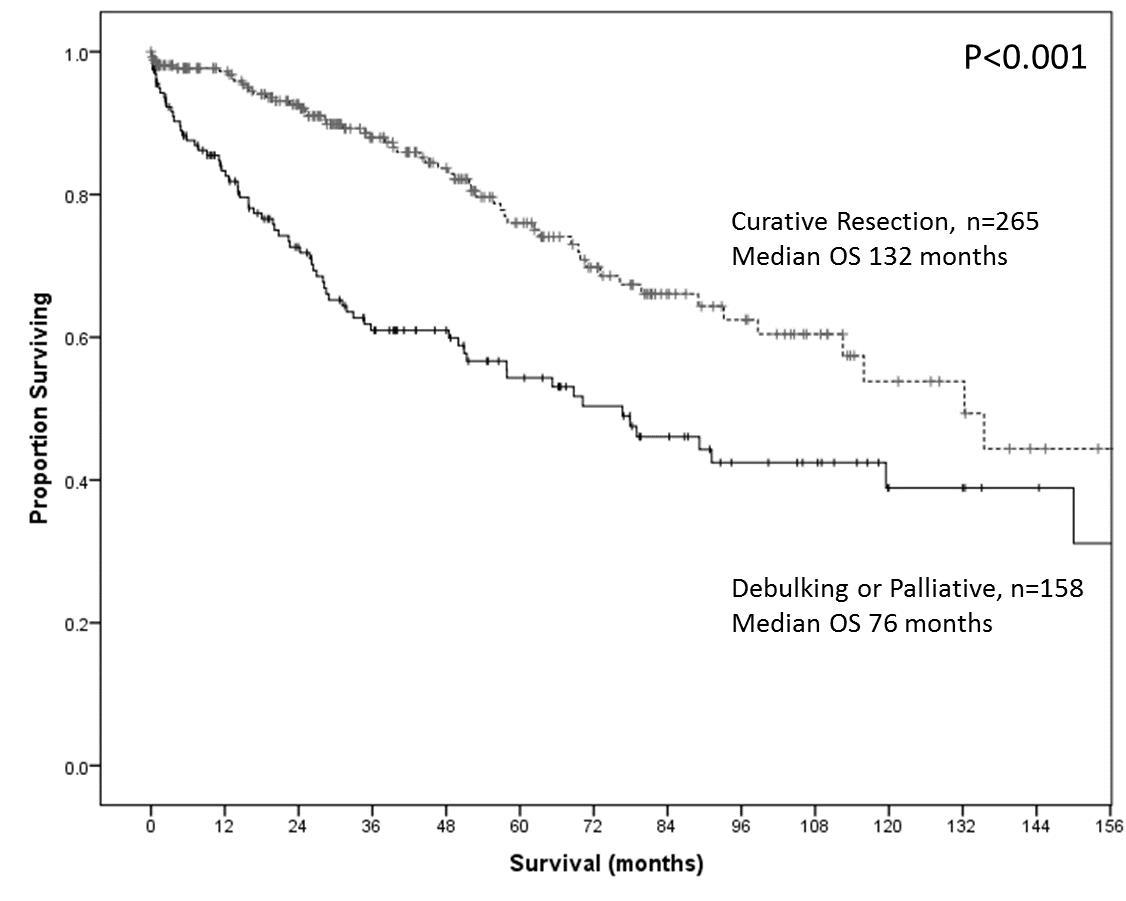
Figure 1: Overall survival of patients with metastatic NET for NH symptoms after curative and non-curative operations
Back to 2018 Program and Abstracts
|