|
 |
Back to 2018 Program and Abstracts
PATIENT CO-MORBIDITY AND FUNCTIONAL STATUS INFLUENCE THE OCCURRENCE OF HOSPITAL ACQUIRED CONDITIONS MORE STRONGLY THAN HOSPITAL FACTORS
Zhobin Moghadamyeghaneh*1, Lygia Stewart1,2
1Surgery, UCSF, San Francisco, CA; 2Surgery, SF VAMC, San Francisco, CA
Objective: Never Events (NE) and Hospital Acquired Conditions (HAC) after surgery are designated as healthcare quality metrics by Medicare and Medicaid Services (CMS) and used as hospital performance measures to dictate payments and penalties. Pre-op patient comorbidity complexity may significantly influence HAC development.
Methods: Using the NIS database 2002-2012, we identified and studied 8,118,615 patients who underwent intra-abdominal gastrointestinal(GI) procedures (Upper/Lower GI and Hepatopancreatobiliary(HPB) procedures). Multivariate analysis, using logistic regression, was used to identify risk factors for HAC and NE following surgery.
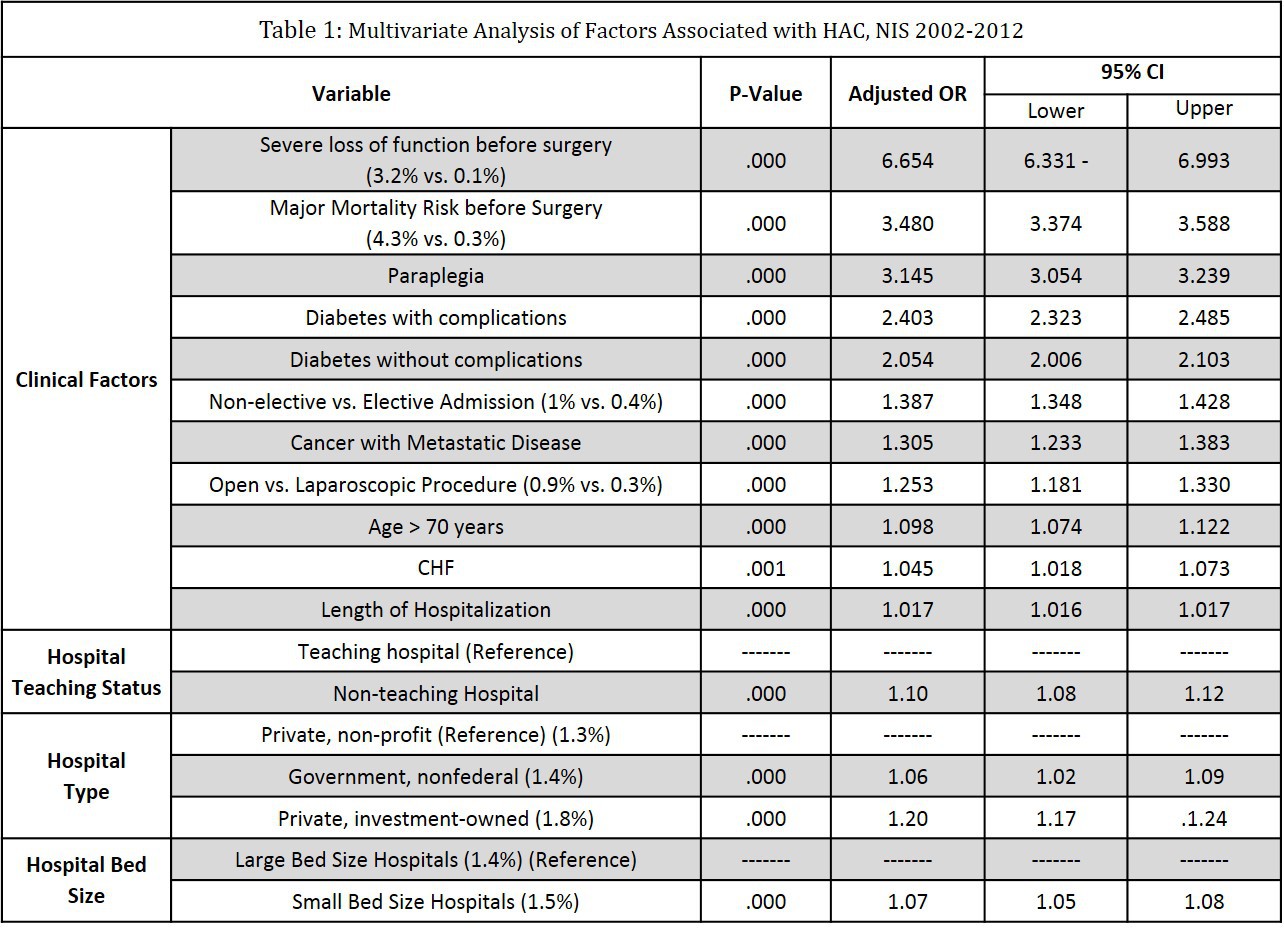
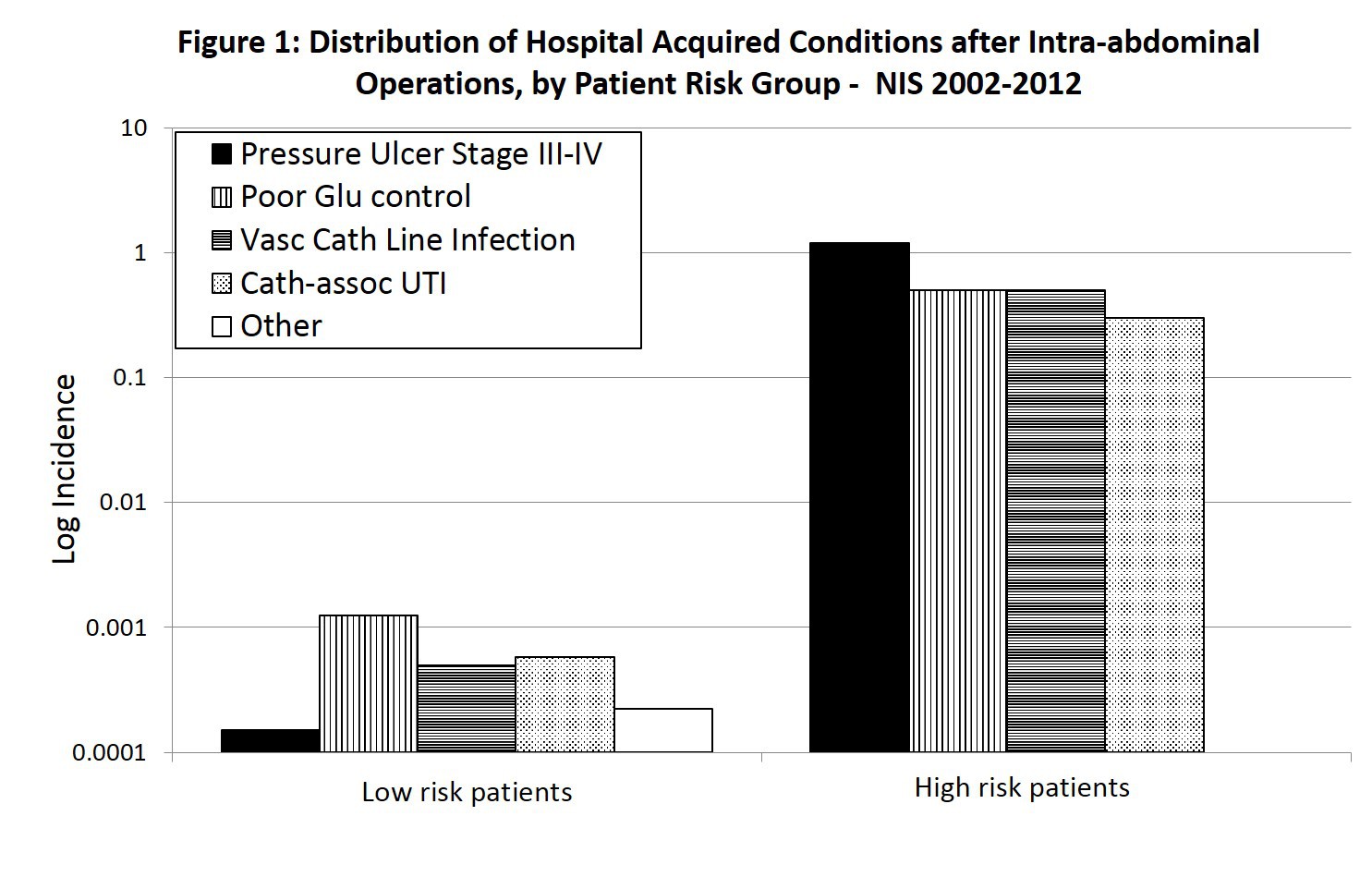
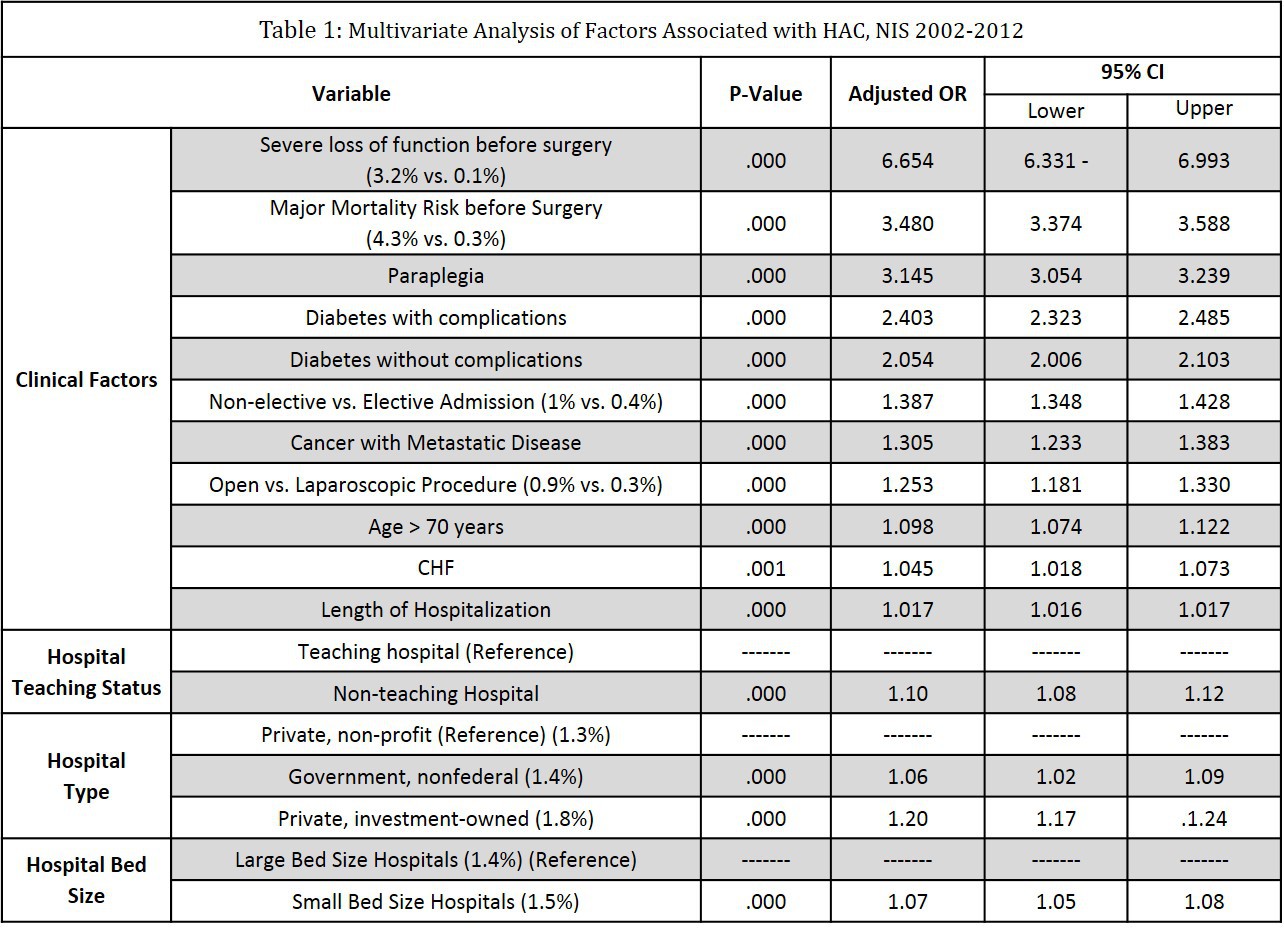
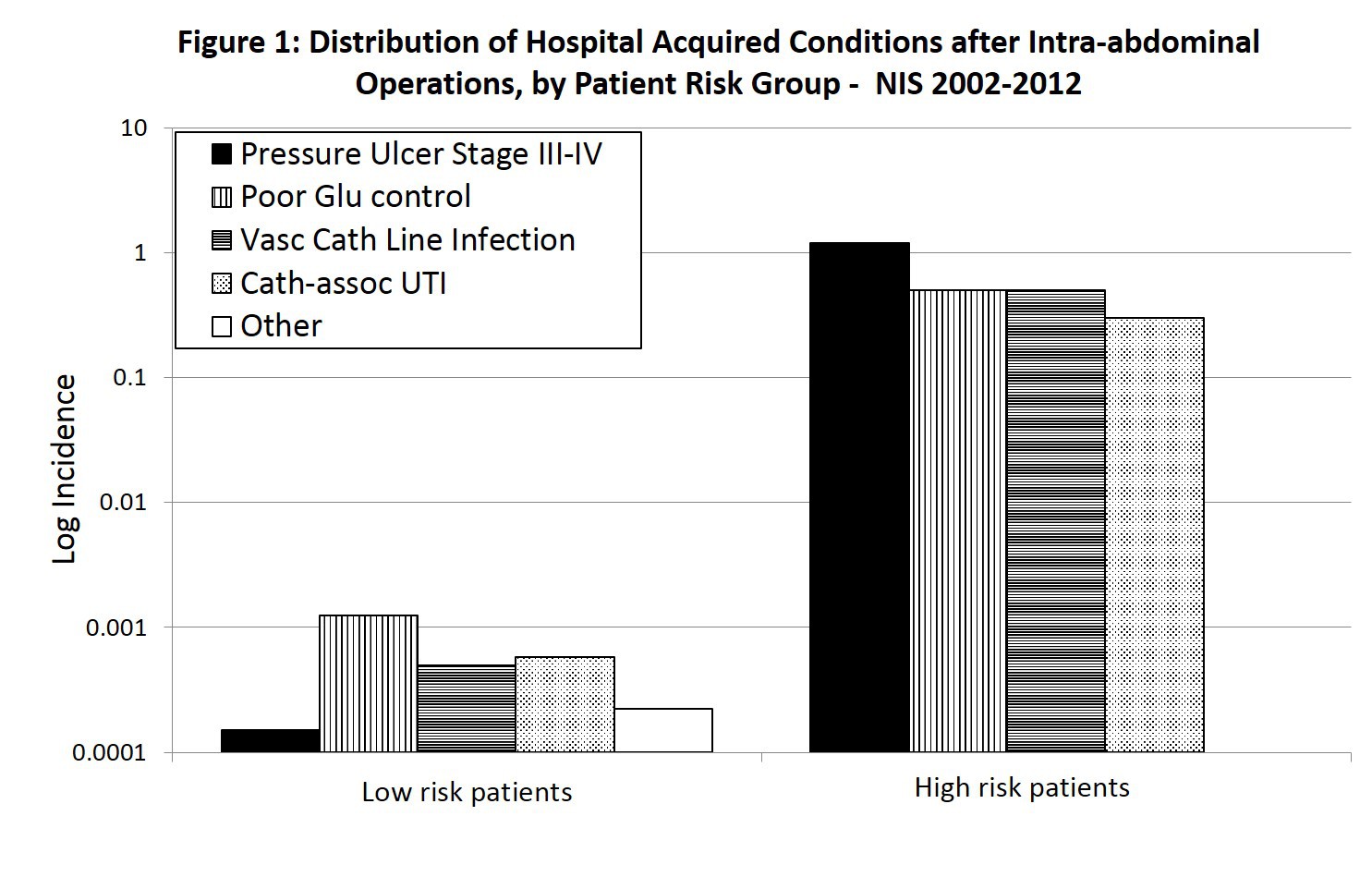
Results: Among 8,118,615 patients, 1645 (0.02%) NE and 63,762 (0.8%) HAC events were reported. Most (99.9%) NE events were retained foreign body. Most frequent HAC events were: pressure ulcer stage III/IV (36.7%), poor glycemic control (26.9%), vascular catheter-associated infection (20.3%), and catheter-associated urinary tract infection (13.7%). HAC were associated with increased mortality (8% vs 2.6%, AOR: 1.14, P<0.01), but not NE (5.3% vs. 2.6%, AOR: 0.86, CI:0.61-1.51,P=0.96). HAC and NE events increased mean length hospitalization (21 vs 7 days,P<0.01), and total hospital charges ($164803 vs. $54858, P<0.01). Several factors increased HAC risk: open vs laparoscopic surgery (0.9% vs. 0.3%, AOR: 1.25,P<0.01), high-risk patients with significant comorbid conditions [severe loss of function pre-op (3.2% vs 0.1%, AOR: 6.65, P<0.01), diabetes with complications (AOR: 2.40,P<0.01), paraplegia (AOR: 3.14,P<0.01), metastatic cancer (AOR: 1.30, P<0.01), age >70 years (AOR: 1.09, P<0.01)], hospital factors [small vs large hospitals (AOR: 1.07, P<0.01), non-teaching hospitals vs teaching hospitals (AOR: 1.10, P<0.01), private profit hospitals vs. non-profit or governmental hospitals (AOR: 1.20, P<0.01)], non-elective admission (AOR: 1.38, P<0.01), and prolonged hospitalization (AOR: 1.01< P<0.01)(Table 1). High-risk patients (with severe comorbid conditions pre-op) had an exponentially higher risk of HAC than low-risk patients (Figure 1 - note, it is a Log plot).
Conclusion: HAC and NE impacted outcomes following intra-abdominal GI operations. The incidence of HAC was higher among patients with severe comorbid conditions. While small, non-teaching, for profit hospitals, and open operations, were associated with increased HAC events; the strongest HAC risk factors were non-modifiable patient factors (preoperative loss of function, severe risk of mortality after surgery, paraplegia, diabetes, metastatic cancer, advanced age, and non-elective admission). This data questions whether HAC are truly hospital performance measures, and suggests that hospitals caring for high-risk complex patients could be unduly penalized. CMS should consider patient comorbidity as a crucial factor influencing HAC development
Back to 2018 Program and Abstracts
|