|
 |
Back to 2018 Program and Abstracts
ONE THOUSAND AND ONE LAPAROSCOPIC HELLER MYOTOMIES FOR ESOPHAGEAL ACHALASIA: TWENTY-FIVE-YEAR EXPERIENCE AT A SINGLE TERTIARY CENTER
Mario Costantini*1, Renato Salvador1, Giovanni Capovilla1, Guerrino Voltarel1, Anna Perazzolo1, Loredana Nicoletti1, Dario Briscolini1, Andrea Costantini2, Lorenzo Vallese1, Stefano Merigliano1
1Surgery, University of Padova, Padova, Italy; 2School of Medicine, Università Cattolica Sacro Cuore, Roma, Roma, Italy
BACKGROUND: In the last decade of the past century, primary Laparoscopic Heller Miotomy (LHM) for achalasia progressively became the procedure of choice in the new millennium. The aim of this study was to assess the long-term outcome of LHM to treat achalasia at a single high-volume institution during the past 25 years.
METHODS: Patients undergoing laparoscopic surgical treatment for esophageal achalasia from 1992 to 2017 were prospectively collected with a dedicated database. Patients who had already been treated were ruled out. Symptoms were collected and scored using a detailed questionnaire; barium swallow, endoscopy, manometry (conventional or HRM) were performed, before and after surgery while, 24-hour pH monitoring were performed 6 months after surgery. Treatment failure was defined as a postoperative symptom score >10th percentile of the preoperative score (i.e. > 8).
RESULTS: 1001 patients underwent LHM by 6 staff surgeons. A partial anterior fundoplication (Dor) was performed in all. They were 536 male and 464 female, their median age was 46 (IQR 36-54; 183 (18.3%) had a history of endoscopic treatments (pneumatic dilation, botox injections, or both). The surgical procedure was completed laparoscopically in all but 7 patients (0.7%) and there was one perioperative death for myocardial infarction.
There were 25 mucosal lesions (2.5%) which was found unrelated to patients' previous treatment, symptom's score, age, radiological-stage, manometric-pattern.
In 674 patients the assessment of the manometric pattern was possible, and was classified as follows: 310 (46%) pattern I, 315 (46.7%) pattern II and 49 (7.3%) pattern III.
The outcome was positive in 903 patients (90.3%). In patients who had a previous treatment the failures were 25/183 (13.7%) while in the primary treatment group the failures were 73/818 (8.9%) (p=0.055). All the 98 patients whose LHM failed subsequently underwent one or more endoscopic pneumatic dilations, which ameliorated their symptoms in all but 11 patients (10 of whom required reoperation). The overall success rate of the combination of LHM and endoscopic dilations was 98.4%.
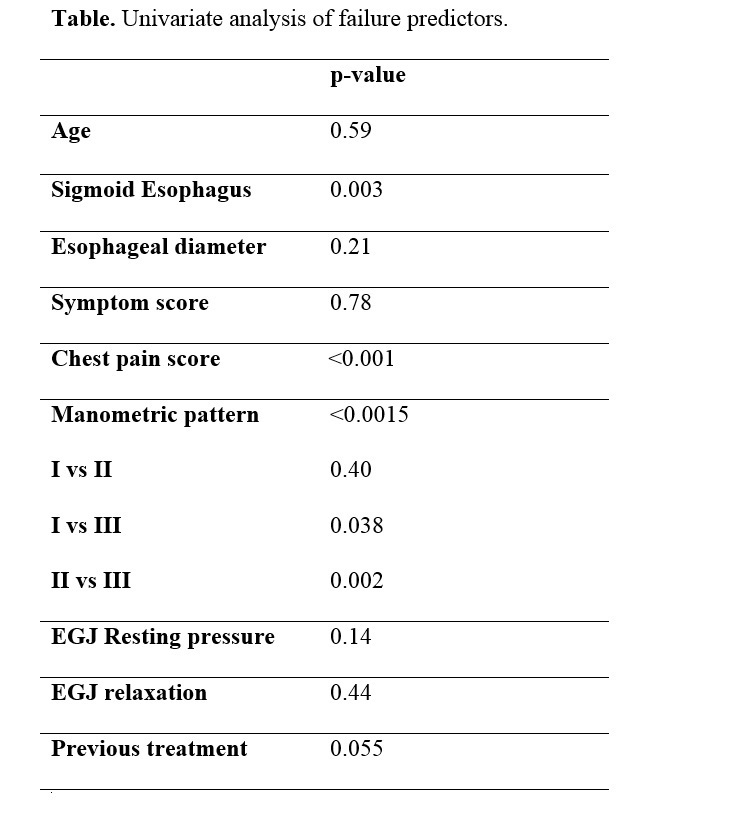
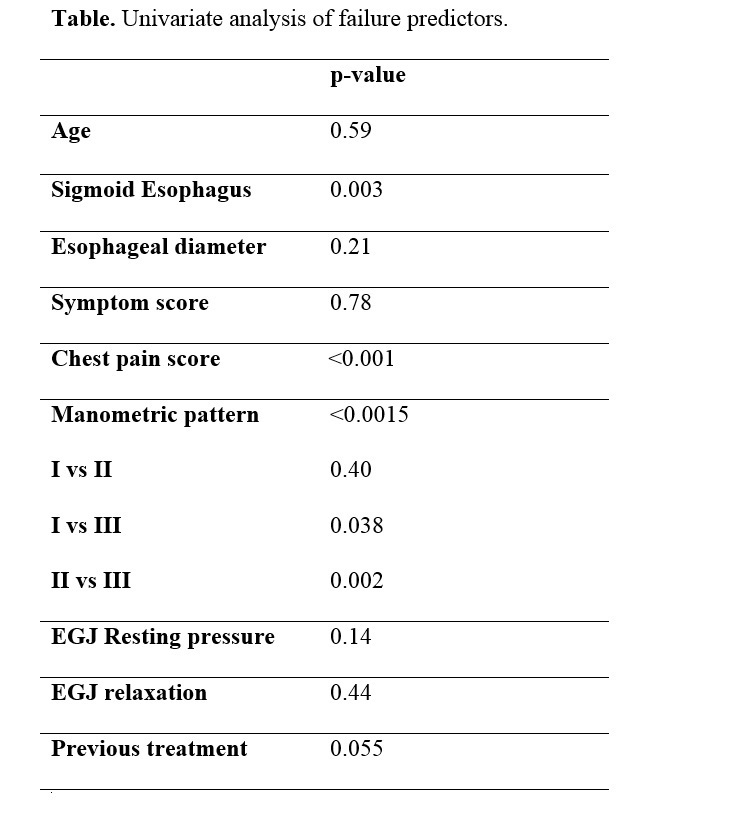
At univariate analysis, the manometric pattern (p=0.0015), the presence of a sigmoid megaesophagus (p=0.003) and the chest pain score (p<0.001) were the only factors predictive of a poor outcome (table). At multivariate analysis, these three factors were independently associated to poor outcome.
Postoperative 24-hour pH-monitoring was abnormal in 50/590 patients (8.5%), and two patients developed an esophageal cancer during the follow-up.
CONCLUSIONS:
LHM can durably relieve achalasia symptoms in about 90% of patients, and recurrence can be successfully treated with complementary dilations in nearly all cases. The preoperative manometric pattern, the presence of a sigmoid esophagus and the chest pain score represent the strongest predictor of outcome.
Back to 2018 Program and Abstracts
|