|
Back to 2018 Program and Abstracts
NEAR INFRARED IMAGING VERSUS PHYSICAL EXAMINATION FOR GASTRIC CONDUIT PERFUSION ASSESMENT DURING MINIMALLY INVASIVE IVOR LEWIS ESOPHAGECTOMY
Mark E. Diebel*1, Lori Gurien1, Brian G. Dalton1, Abubaker Ali2, Ziad Awad1
1Surgery, University of Florida Jacksonville, Jacksonville, FL; 2Surgery, Wayne State University, Detroit, MI
Objective: The goal of this study was to evaluate the ability of intraoperative near infrared perfusion assessment of the gastric conduit to identify an at-risk esophagogastrostomy performed during a minimally invasive esophagectomy (MIE). Furthermore, we sought to compare it as a qualitative study to physical examination of the gastric conduit.
Esophagectomy is the most technically demanding operation in foregut surgery. The majority of the morbidity and mortality associated with esophagectomy is related to anastomotic leak, with ischemia often resulting in this dreaded complication. Near infrared imaging (NIR) allows for real time assessment of tissue perfusion. We hypothesized that poor perfusion as suggested by NIR would predict an at-risk esophagogastrostomy, and that in MIE, it would be a superior qualitative test as compared to physical exam.
Methods: A retrospective study of prospectively collected data from 2014-2017 of 66 consecutive MIE was performed with intraoperative gastric conduit perfusion assessment using NIR laparoscopic system (PINPOINT). All operations were performed by a single surgeon at a tertiary referral center via a minimally invasive Ivor-Lewis technique. PINPOINT assessment of the gastric conduit was performed intra-abdominally following gastric conduit tubularization, and intrathoracically following creation of esophagogastrostomy. Surgical technique modification was guided by PINPOINT and correlation with physical exam was determined. Factors associated with esophageal leak and for expected leaks based on PINPOINT were analyzed using chi-square tests.
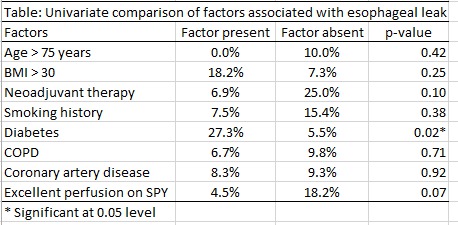
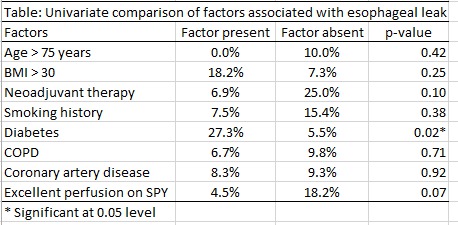
Results: The average age of this patient population was 65 years old, and 83% were male. The mean BMI was 26.2 kg/m2. 79% of these patients were diagnosed with adenocarcinoma, and 94% (60/64) of the patients with a cancer diagnosis underwent neoadjuvant chemoradiation. Associated comorbid conditions were as follows; COPD (23%), diabetes (17%), coronary artery disease (18%), and smoking history (80%). Routine esophagram was obtained on POD 4, which demonstrated anastomotic leak in 3 patients. 6 anastomotic leaks were diagnosed and managed endoscopically via stent placement. There were no mortalities at 30 days. Diabetes was the only statistically significant risk factor for anastomotic leak (p=0.02). Near infrared imaging suggested poor perfusion in 22 studies. Surgical technique was modified in all of these and only 6 leaks were observed, which was significantly less than the 22 predicted by PINPOINT(p<0.0001).
Conclusion: Poor perfusion based on PINPOINT was not a statistically relevant risk factor for anastomotic leak, yet surgical technique was modified; therefore, this data suggests that poor perfusion on PINPOINT can identify an at-risk anastomosis. In addition, PINPOINT compared to physical exam appears to be a superior qualitative examination of the gastric conduit

Back to 2018 Program and Abstracts
|