|
Back to 2018 Program and Abstracts
THE PROGNOSTIC SIGNIFICANCE OF THE NUMBER OF METASTATIC LYMPH NODES IN GASTRIC NEUROENDOCRINE TUMORS
Linda M. Pak*1,2, Tingsong Yang1, Jiping Wang1,2
1Surgery, Brigham and Women's Hospital, Boston, MA; 2Center for Surgery and Public Health, Brigham and Women's Hospital, Boston, MA
BACKGROUND: For gastric neuroendocrine tumors (GNET), the current American Joint Committee on Cancer (AJCC) lymph node (N) stage classifies patients into N0/N1 disease (with/without lymph node metastases); however, this does not adequately account for the prognostic impact of the number of metastatic nodes. The objective of this study was to develop and validate a new nodal classification system for GNET based on the number of metastatic lymph nodes.
METHODS: The National Cancer Database (NCDB) was queried from 2004 to 2014 for all patients with GNET who had undergone partial or total gastrectomy with known nodal status. Nearest neighborhood grouping was used to identify survival clusters by number of metastatic lymph nodes and to use these groupings to construct a new N classification system. Kaplan-Meier survival curves were used to compare overall survival (OS) among the new N classification groups. Multivariable Cox regression analysis was used to identify patient and disease characteristics independently associated with OS. The proposed N classification (pN) was subsequently validated using the Surveillance, Epidemiology, and End Results (SEER) database (1998-2013).
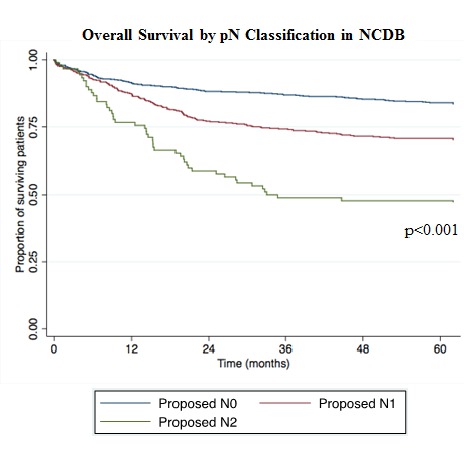
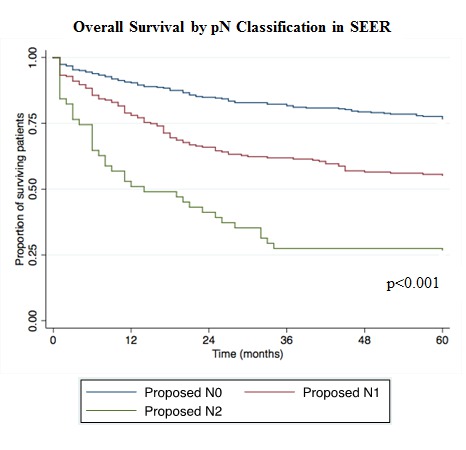
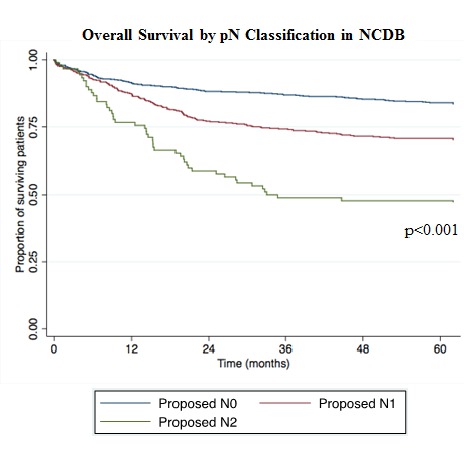
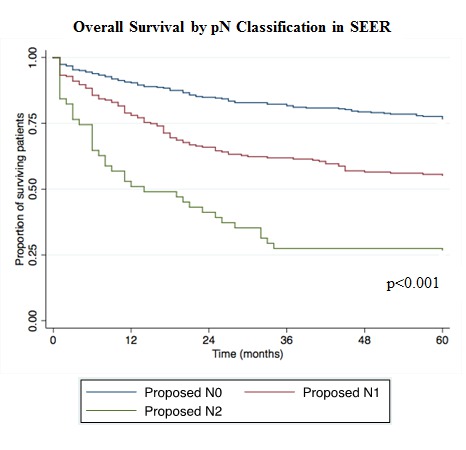
RESULTS: In the NCDB, 1,275 patients met study inclusion criteria. In addition to patients with no lymph node metastases (pN0), patients with 1-6 positive lymph nodes (pN1) demonstrated a distinct survival pattern from patients with ≥7 positive lymph nodes (pN2) [5-year OS 80% (95%CI 77-83%) vs 65% (95%CI 61-69%) vs 43% (95%CI 33-53%), p<0.001] (Figure 1). Patients with pN2 disease also presented with distinct histopathologic features from pN1 patients, including larger primary tumors with poor differentiation, higher T stage, and presence of lymphovascular invasion (p=0.001-0.004). Using the SEER database, the pN classification continued to demonstrate strong discriminatory ability in differentiating survival outcomes among pN0/pN1/pN2 patients [5-year OS 70% (95%CI 65-75%) vs 53% (95%CI 46-59%) vs 18% (95%CI 9-29%), p<0.001] (Figure 2). On multivariable analysis, male sex, tumor location in the body of the stomach, poor/undifferentiated tumors, T4 tumors, and pN2 disease remained significantly associated with OS.
CONCLUSIONS: The number of metastatic lymph nodes is an independent prognostic factor for patients with GNET; current AJCC N1 disease contains patients with heterogeneous prognosis. In particular, the presence of ≥7 positive lymph nodes was significantly associated with poorer survival compared to 1-6 positive nodes.
Back to 2018 Program and Abstracts
|