|
Back to 2018 Program and Abstracts
DOES THE MFI SCORE PREDICT MORBIDITY AND MORTALITY AFTER GASTRECTOMY FOR NON-BARIATRIC DISEASE?
Konstantinos Zorbas*3, Vic Velanovich2, Sanjay S. Reddy3, Nestor Esnaola3, Andreas Karachristos1,3
1Surgical Department, Temple University Hospital, Philadelphia, PA; 2Surgery, University of South Florida, TAMPA, FL; 3Department of Surgical Oncology, Fox Chase Cancer Center, Philadelphia, PA
Objective(s)
The modified frailty index (MFI) has been studied and proven to be associated with mortality and morbidity after major operations like pancreatectomies and liver resections. The aim of our study was to validate MFI as a preoperative risk predictor for postoperative morbidity and mortality after gastrectomy for non-bariatric disease.
Methods
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database was queried for patients who underwent total or partial gastrectomy for malignant or benign disease from 2005 to 2011. The MFI was calculated, based on 11 variables: functional status; diabetes mellitus (DM); chronic obstructive pulmonary disease (COPD) or pneumonia; congestive heart failure (CHF); previous myocardial infarction (MI); previous percutaneous coronary intervention (PCI), cardiac surgery, or angina; hypertension (HTN) requiring the use of medications; peripheral vascular disease or rest pain; impaired sensorium; history of transient ischemic attacks (TIA) or cerebrovascular accident without residual deficit; and history of cerebrovascular accident with residual deficit. The population was then divided into four categories based on the MFI score. Thirty-day mortality, postoperative complications, and failure to rescue rate were evaluated. Chi-square test, logistic regression analyses and other tests were used to evaluate the four frailty groups.
Results
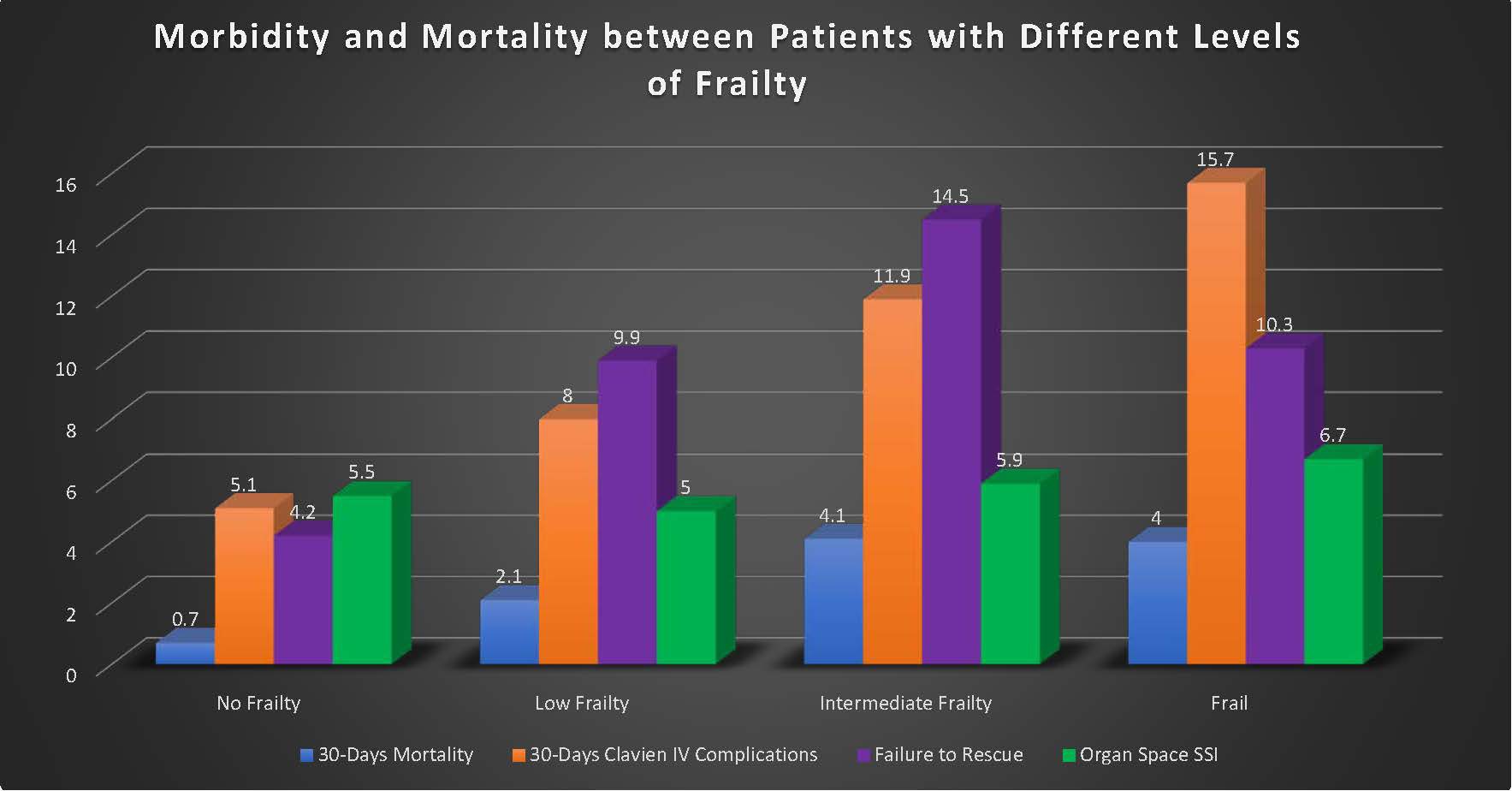
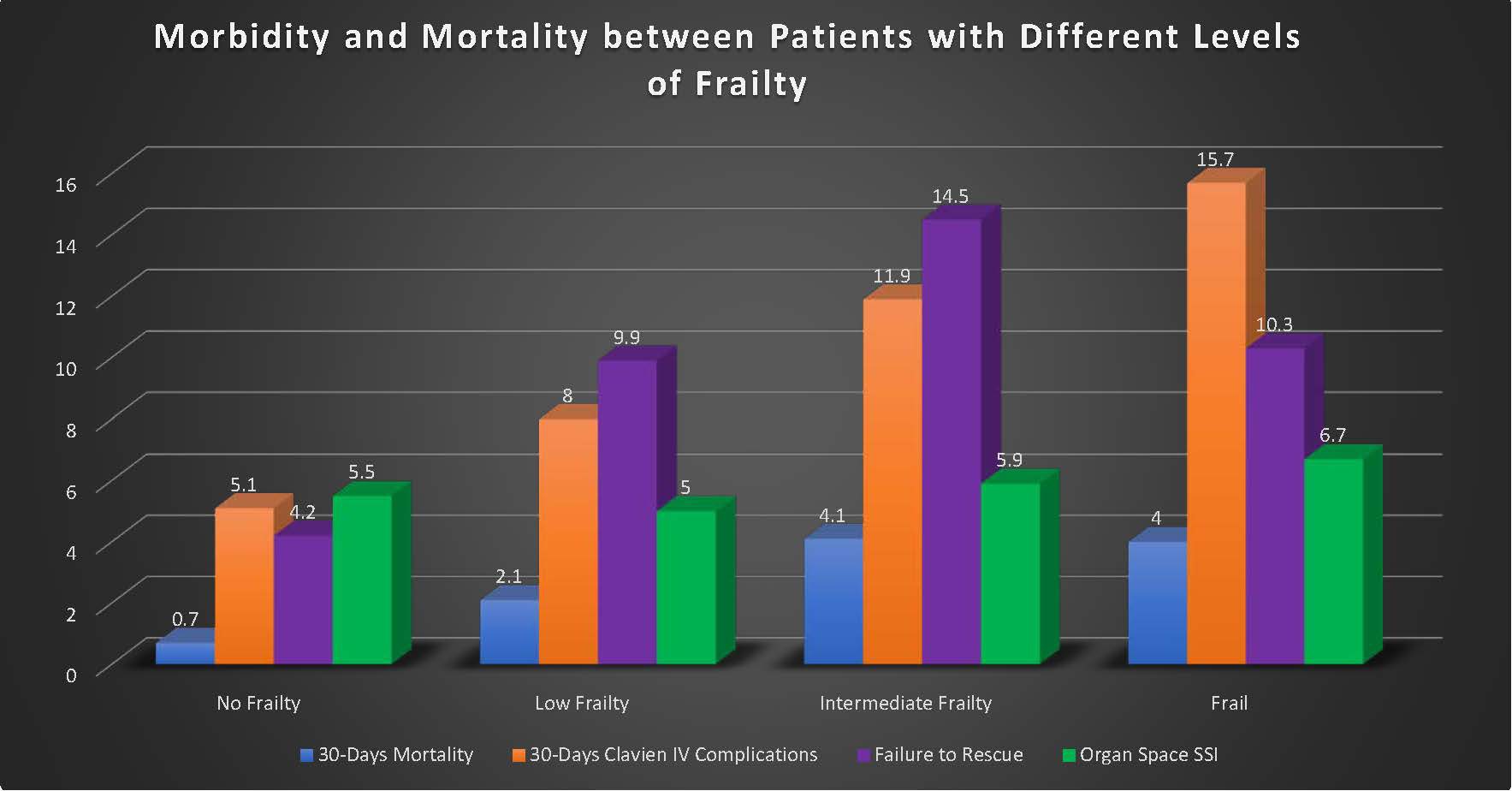
Overall, 4,961 patients underwent a gastrectomy for non-bariatric disease. There were 1,907 (38.4 %) patients with no frailty, 1,713 (34.5 %) patient with low frailty (MFI=1), 921 (18.6 %) with intermediate frailty (MFI=2), and 420 (8.5%) frail patients (mFI≥3). An MFI score of ≥2 was associated with significantly higher odds of postoperative mortality, from 0.7 % in the non-frail group, to 4% in the intermediate frailty and frail groups). There were higher odds of having a serious postoperative complication from 5.1% in the non-frail group, to 15.7 % in the frail group. There were higher odds of failure to rescue after a serious postoperative complication from 4.2 % in the group with a 0 MFI score, to 14.5 % in those with an MFI score of 2.
Conclusion
An increasing MFI score in patients undergoing non-bariatric gastrectomy is associated with a higher incidence of morbidity, mortality, and failure to rescue after a serious complication. This frailty score can be easily calculated preoperatively from patient's history and it can be used as a useful adjunct for operative treatment planning.
Back to 2018 Program and Abstracts
|