|
Back to 2018 Program and Abstracts
TIMING AND PATTERN OF RECURRENCE FOLLOWING ESOPHAGECTOMY FOR ESOPHAGEAL CARCINOMA
Melissa L. DeSouza*, Sabrina E. Drexel, Elizabeth Dewey, John G. Hunter, Nadine Mallak, James P. Dolan
General Surgery, Oregon Health & Science University, Portland, OR
Background: In the United States, esophagectomy continues to be an important modality in the curative treatment of esophageal cancer. Increased overall survival has been demonstrated when surgery is performed following chemoradiotherapy. Despite this, the risk of recurrent malignancy remains a concern. Currently, no specific recommendations exist regarding the frequency or duration of cross-sectional imaging for surveillance. The aim of this study was to determine the timing and pattern of cancer recurrence following esophagectomy in order to guide an optimal surveillance program.
Methods: We performed a retrospective review of a prospectively-maintained esophageal disease registry from an NCI-designated Comprehensive Cancer Center. Patients who underwent esophagectomy for cancer between 2000 and 2017 were included. Our institutional surveillance protocol consists of computed tomography (CT) scanning every 3-months for the first year, every 6-months for the 2nd year, then annually from the 3rd year forward until the 5th year postoperatively. Rates of tumor recurrence were assessed using chi-square tests. Monthly recurrence rate and overall survival were assessed using Kaplan-Meier analysis. Risk ratios for recurrence were evaluated with a multivariate Cox regression model.
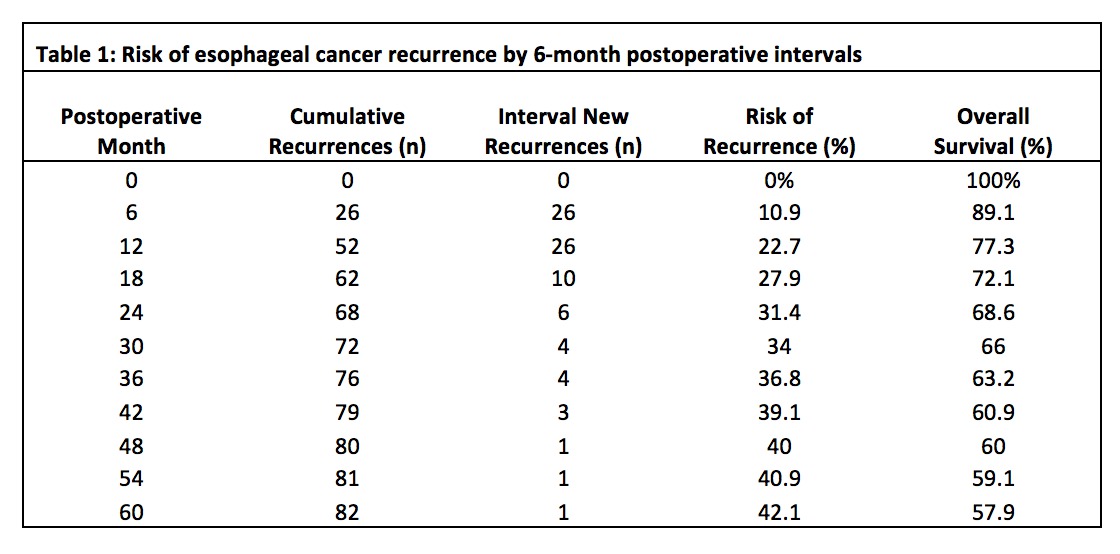
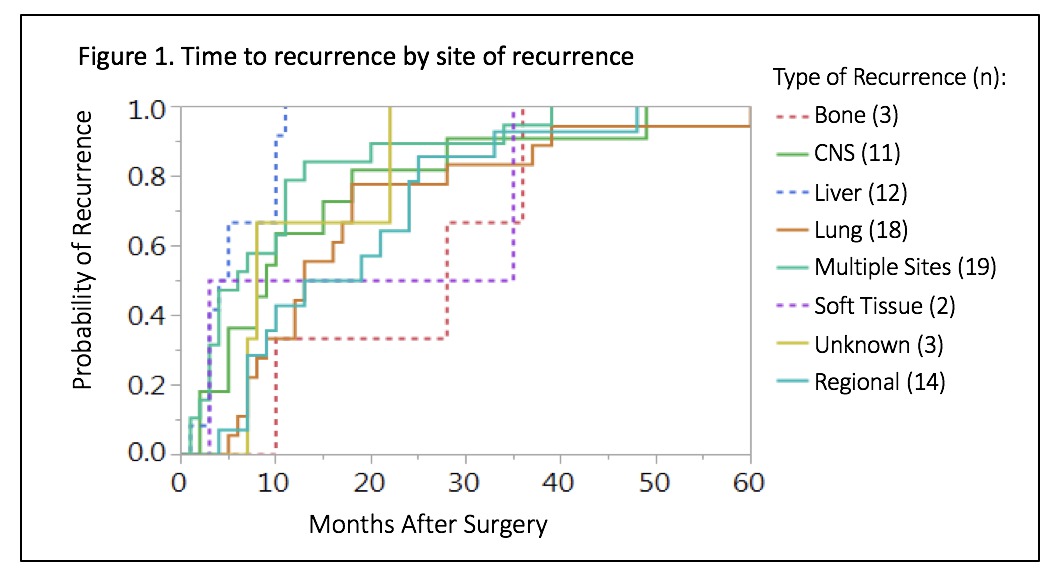
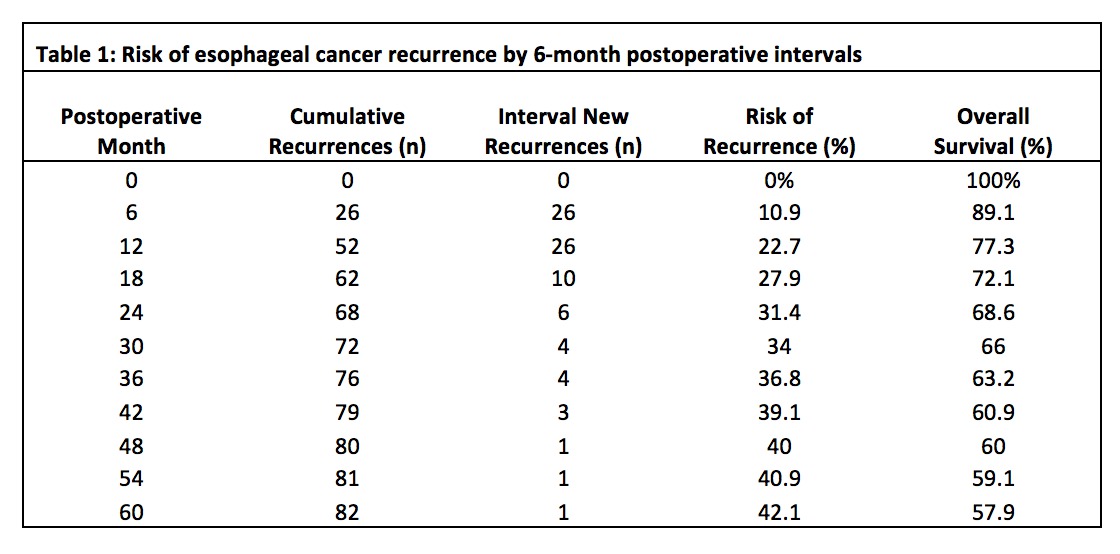
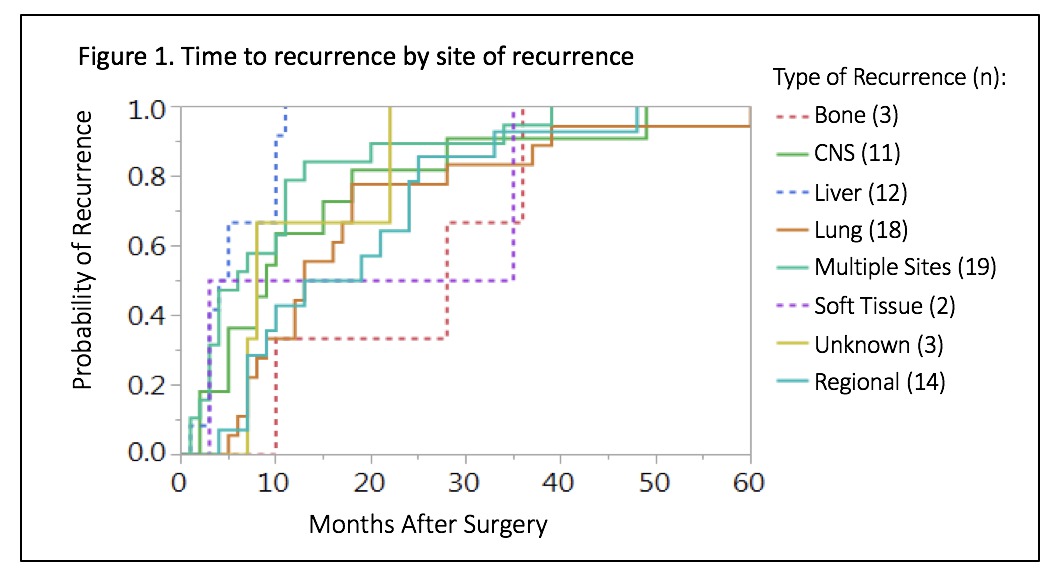
Results: A total of 273 patients were included, 84% were male and 96% Caucasian. Adenocarcinoma was the most common subtype (88%). Patients with microscopic residual disease at resection margins were excluded from recurrence analysis (n=19). Of the remaining 254 patients, 81% received chemotherapy and 77% received radiation. The overall rate of recurrence was 32%. There was an increased likelihood of recurrence in patients with higher stage disease (Stage 3 vs Stage 2 RR: 3.7, p<0.0001, and Stage 3 vs Stage 1 RR: 5.26, p=0.04). Half of all patients had symptoms at the time of clinical recurrence (49%) but a majority were diagnosed with recurrent disease by routine surveillance imaging (59%). Eighty-three percent of recurrences occurred within the first 2 years, with more interval recurrences occurring at the 6- and 12-month marks (Table 1). After 24 months, there was a notable decrease in annual recurrence rates. Most recurrence was multi-site (25.3%), followed by lung (22.7%) and regional (18.7%) recurrence. There were notable differences in time to recurrence by site of recurrence (p=0.0093)(Figure 1).
Conclusions: In our population, 32% of patients had recurrence of esophageal cancer following esophagectomy. Highest risk of recurrence was within the first 2 postoperative years, followed by a steep annual decline in recurrence rates. These findings favor the practice of more frequent CT surveillance in the first 2 years, followed by annual surveillance. We also noted isolated liver recurrence presented sooner compared to more distant recurrence within our population.
Back to 2018 Program and Abstracts
|