|
 |
Back to 2017 Posters
THERAPEUTIC STRATEGIES FOR SEVERE AND SEVERE-COMPLICATED CLOSTRIDIUM DIFFICILE INFECTION.
Reema Mallick1, Victor Vakayil*1, Amanda Lord1, Patrick McGonagill1, Malavika Chandrashekar1, Osama Alsaied1, Wolfgang B. Gaertner1, Alexander Khoruts2, James Harmon1
1Surgery, University Of Minnesota, Minneapolis, MN; 2Gastroenterology, University Of Minnesota, Minneapolis, MN
Background: The management of severe and severe-complicated Clostridium difficile infection (CDI) is challenging and continues to be associated with high mortality. Despite high mortality rates of up to 50% at 30 days, total abdominal colectomy remains the standard of care. However, novel therapeutic interventions including loop ileostomy with antegrade irrigation and fecal microbiota transplantation (FMT) appear to be promising alternatives to the treatment of severe and severe-complicated CDI.
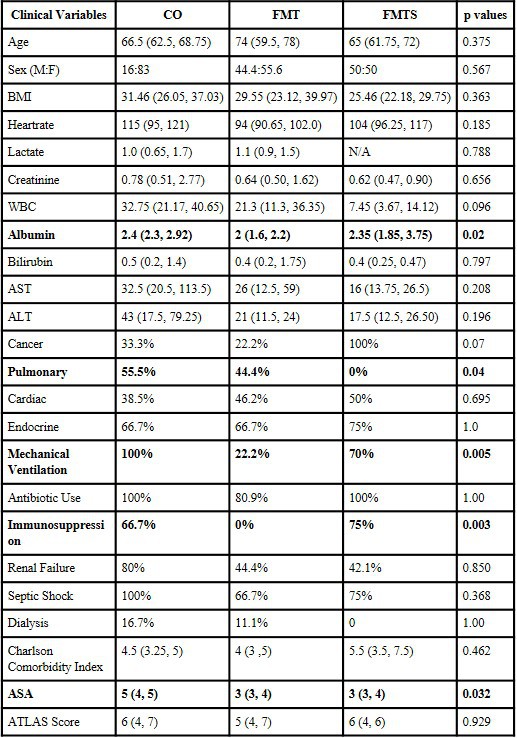
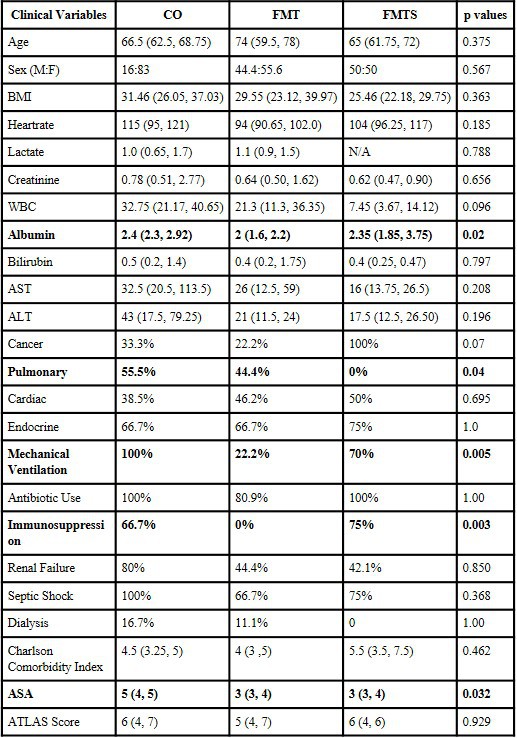
Methods: Single-center, retrospective review was performed of all patients diagnosed with CDI at our hospital from 2008-2016. All cases of severe and severe-complicated CDI that underwent total abdominal colectomy or FMT were identified. This yielded three cohorts: 1. Total abdominal colectomy alone (CO), 2. FMT alone (FMT), and 3. Initial FMT followed by total abdominal colectomy for refractory disease (FMTS). Patient demographics, history, comorbidities, clinical and laboratory variables, ATLAS CDI severity scores, hospital/ICU stays, procedural information, and 30-day and 60-day mortality outcomes were analyzed.
Results: 5,150 patients were identified to have a CDI from 2008-2016 and 19 of these patients (CO-6, FMT-9, FMTS-4) were included in this study. Patient demographics and ATLAS CDI severity scores were comparable but comorbidity profiles differed (Table 1). The median number of FMTs in the FMT group was 2 (IQR 1,3) and 1.5 (IQR 1,2) for the FMTS group. The 30-day mortality rates for the CO, FMT, and FMTS groups were 33.3%, 22.2% and 25%, respectively, while the 60-day mortality rates for the CO and FMT groups increased to 50% and 33.3% (p=0.097, 0.312), respectively. The observed mortality rate (OMR) from the ATLAS score compared to the predicted mortality rate (PMR) was statistically significant for the CO group only (PMR 11% vs. OMR 50%, p=0.002). For the FMT and FMTS groups, there were no significant differences between OMR and PMR (p>0.05).
Conclusion: Patients who underwent surgery for severe and severe-complicated CDI had high mortality. Selective patients who underwent FMT with or without subsequent surgical intervention had decreased 30- and 60-day mortality compared to surgery alone. Although these outcomes likely represent differences in disease severity and patient-related factors, FMT may impact outcomes in selective patients with severe and severe-complicated CDI even if given before surgery. Despite our small sample size, these results merit further inquiry into the effect of early FMT in patients with severe and severe-complicated CDI.
Back to 2017 Posters
|