|
Back to 2017 Posters
ENHANCED RECOVERY PATHWAY USE REDUCES POSTOPERATIVE ILEUS AFTER ILEOSTOMY CLOSURE
Michael Deutsch, Hae Soo Joung, Prashant Sinha, Paresh C. Shah*
Surgery, NYU Langone Medical Center, New York, NY
Introduction: Postoperative ileus (POI) following loop ileostomy closure is a common and persistent problem which can prolong hospitalization. Enhanced Recovery Pathway (ERP) use has been demonstrated to improve peri-operative outcomes after colo-rectal resections. We sought to identify whether the systemic implementation of an ERP would also improve outcomes after ileostomy closure. This study reports the experience of a high volume, quaternary care, academic medical center where >70% of primary colo-rectal surgery is performed using laparoscopic or robotic techniques.
Methods: All adult patients undergoing elective ileostomy closure at our center from 1/1/2013 through 5/31/2016 were reviewed. Cases with multiple major procedures, ileo-colonic anastomosis and incomplete medical record data were excluded. Closure technique was per surgeon preference. Pre-and post-operative variables were captured as part of our ERP monitoring program. Postoperative ileus was defined as (re)placement of a nasogastric tube in the postop period, no bowel function for more than 6 days, or diet cessation due to distension. An ERP for elective colo-rectal surgery was implemented at our institution in 3/2015. Outcome variables assessed included postoperative ileus (POI), time to diet, time to flatus, length of stay, mortality, 30 day readmission, and reoperation.
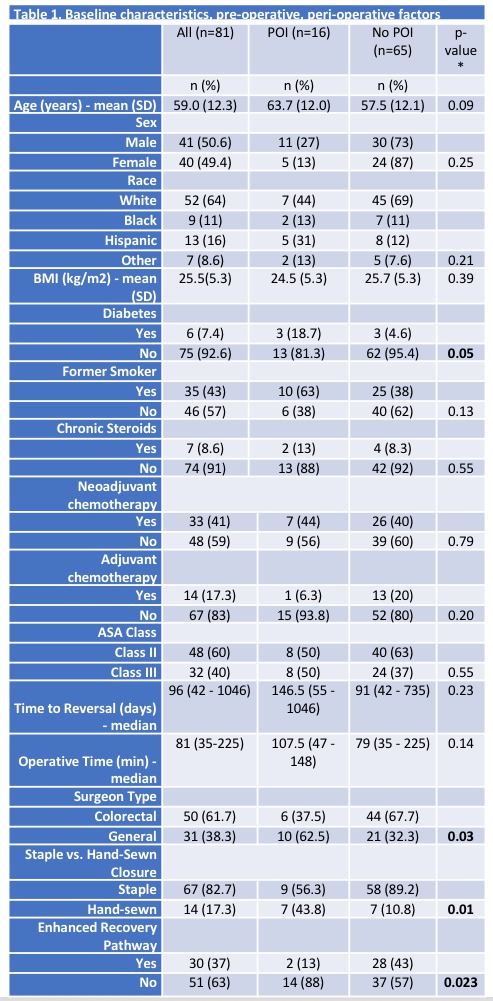
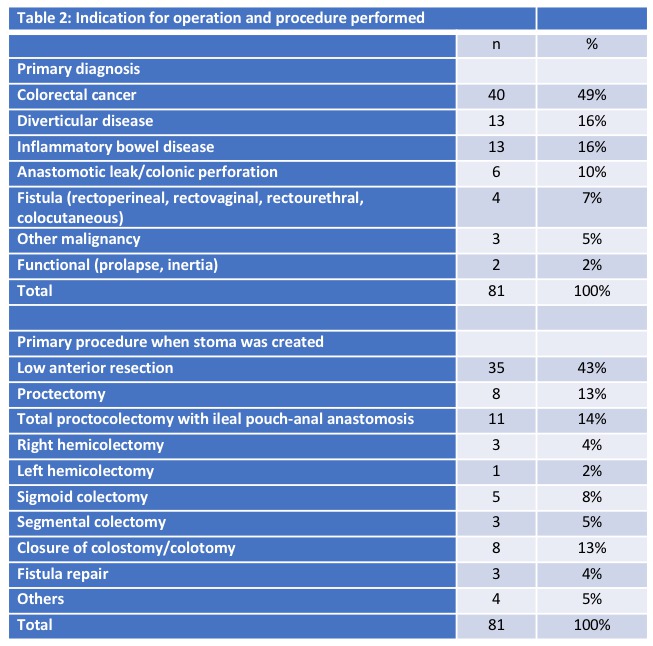
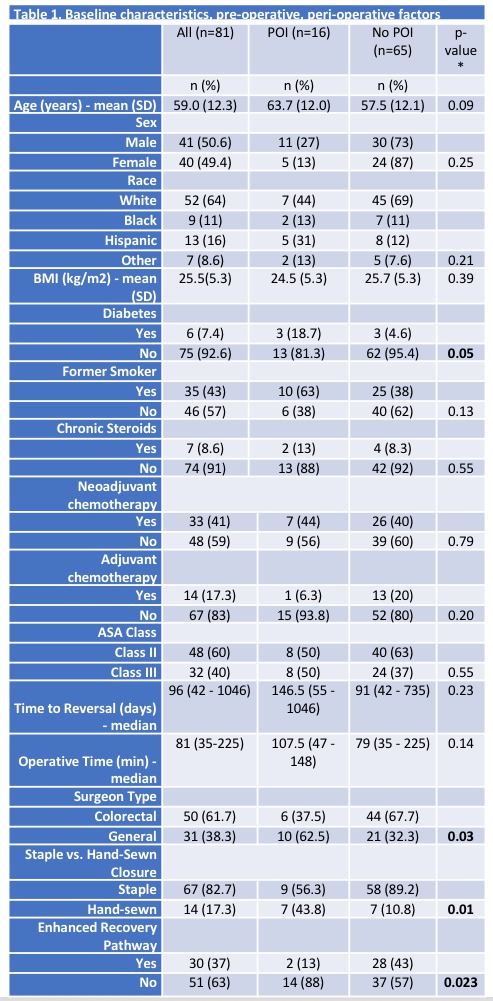
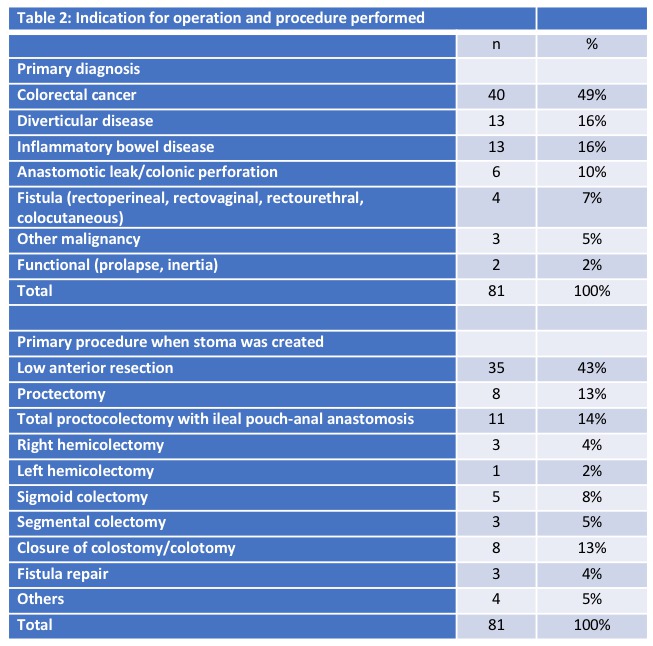
Results: Eighty-one patients were identified who met the inclusion criteria. There were 41 males and 40 females. Demographic variables are detailed in Table 1. The most common diagnosis was colorectal cancer (49%) and the most common ileostomy creation procedure was a low anterior resection with ileostomy (43%) (Table 2). Ileostomy reversal was performed after a median interval of 96 days. Median operative time was 81 minutes, and 82.7% (n=67) were stapled closure while 17.3% (n=14) were hand-sewn. POI occurred in 19.8% (16) of patients. POI was seen more often in diabetics (50% vs 17%, p=0.05) and in hand-sewn closure (50% vs 13%, p=0.001). POI was significantly reduced in the ERP era (after 3/2015) than before (7% ERP era, vs 33% before ERP, p=0.003). POI was lower when the ERP order set was used (7% with ERP vs 27% no ERP, p=0.023). Length of stay was shorter with ERP (3.1±1.8 vs 5.0±4.5, p=0.026). The readmission rate was higher in the POI (31% vs 8%, p=0.01). Re-operation was 2.5% (n=2) for anastomotic leak, with one death.
Conclusions: Implementation of an Enhanced Recovery Pathway significantly improves POI after ileostomy closure. Diabetes and technical factors ( sutured vs stapled ) may increase the risk of POI, however the effect of the ERP appears to improve outcomes even in those patients. The effect may be cumulative from the index procedure as well as the ileostomy closure itself.
Back to 2017 Posters
|