|
Back to 2017 Posters
MINIMALLY INVASIVE VERSUS OPEN RESECTION OF ADVANCED GALLBLADDER CANCER: A NATIONAL ASSESSMENT OF SHORT AND LONG-TERM OUTCOMES
Gyulnara G. Kasumova*, Omidreza Tabatabaie, Ayotunde B. Fadayomi, Promise O. Ukandu, Sing Chau Ng, Amy Evenson, Khalid Khwaja, Jennifer F. Tseng
Surgery, Beth Israel Deaconess Medical Center, Boston, MA
Background: Laparoscopic cholecystectomy has been deemed oncologically safe for early stage (pT0 and pT1) gallbladder cancers. However, results surrounding the use of minimally invasive techniques for pT2 and pT3 tumors have been inconclusive. This study aims to evaluate short- and long-term outcomes for patients undergoing minimally invasive versus open resection.
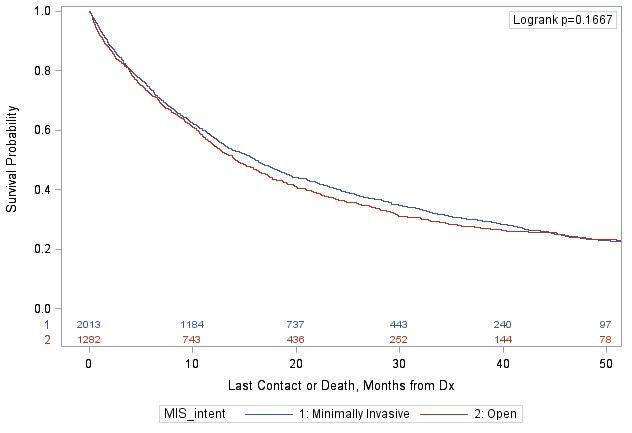
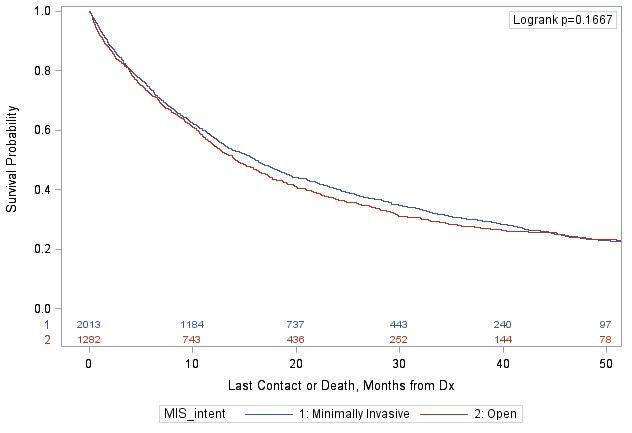
Methods: The National Cancer Data Base was queried for patients with pathologic T2/T3 gallbladder adenocarcinoma diagnosed between 2010-2014 who underwent resection. Minimally invasive surgery was comprised of laparoscopic and robotic assisted cases with intention to treat analysis. Chi-square tests were used to compare patient characteristics and outcomes. Kaplan-Meier method was used to compare overall survival. Sensitivity analyses were performed to evaluate the effect of pT stage and resection type on survival.
Results: A total of 4,210 patients were identified, of whom 61.7% (2,596) had a minimally invasive procedure and 38.3% (1,614) had an open procedure. Of those undergoing a minimally invasive approach, 21.2% (550) required a conversion to open. The majority of patients were female (69.6%), and females were more likely to have an MIS approach (70.8% vs 67.6%; p=0.0280). Patients more likely to have an MIS procedure were also: older than age 70 (58.7% vs 46.4%; p<0.0001), white (80.6% vs 75.3%; p=0.0002), treated mostly at community centers (76.4% vs 58.8%; p<0.0001), and more likely to have pT2 disease (63.0% vs 49.1%; p<0.0001). Patients who underwent a minimally invasive resection had lower 30-day mortality (6.0% vs 8.5%; p=0.0059) and 90-day mortality (15.7% vs 18.4%; p=0.0409), but no difference in unplanned 30 day readmissions (6.9% vs 7.9%; p=0.2369). There was no difference in overall survival between minimally invasive vs open procedure (median 16.1 vs 14.2 months; p=0.1667). These findings remained robust on sensitivity analyses by pT stage and resection type (simple versus extended/radical cholecystectomy).
Conclusions: Minimally invasive approach has a slightly lower perioperative morality relative to open procedures, and it is oncologically safe for patients with pT2 and pT3 tumors and should be considered in patients who are eligible surgical candidates.
Back to 2017 Posters
|