|
 |
Back to 2017 Posters
REOPERATION INCREASES THE INPATIENT MORTALITY IN PANCREATIC CANCER PATIENTS
Chiranjeevi Gadiparthi*1, Rosann Cholankeril1, Eddie L. Copelin2, Eric R. Yoo3, Muhammad Ali Khan1, Menghan Hu5, Aijaz Ahmed4, Colin W. Howden1, George Cholankeril1, Ponnandai Somasundar6
1Department of Gastroenterology and Hepatology, University of Tennessee Health Sciences Center, Memphis, TN; 2Department of medicine, Boston university school of medicine, Boston, MA; 3Department of medicine, University Illinois School of Medicine, Chicago, IL; 4Department of Gastroenterology and Hepatology, Stanford University, Stanford, CA; 5Department of Biostatistics, Brown University School of Public Health, Provide, RI; 6Department of Surgical Oncology, Roger Williams Medical Center, Providence, RI
Background and Aims
Over the last two decades, long-term survival rates after surgical resection for pancreatic cancer have markedly improved. However, postoperative inpatient mortality among patients with resected pancreatic cancer is yet to be assessed. We aim to evaluate temporal trends and predictive risk factors associated with inpatient mortality in patients with resected pancreatic cancer.
Methods
Using the Healthcare Utilization Project-National Inpatient Sample (HCUP-NIS), we evaluated temporal trends and independent risk factors associated with postoperative inpatient morality in resected pancreatic cancer patients from 2004 to 2013. Inclusion criteria were patients with a primary diagnosis of pancreatic cancer who underwent pancreatic resection. Additionally, we performed a multivariate logistic regression analysis assessing risk factors including demographics (age, gender, ethnicity, insurance type), postoperative complications and clinical comorbidities associated with postoperative inpatient mortality in patients who underwent surgical resection for pancreatic cancer.
Results
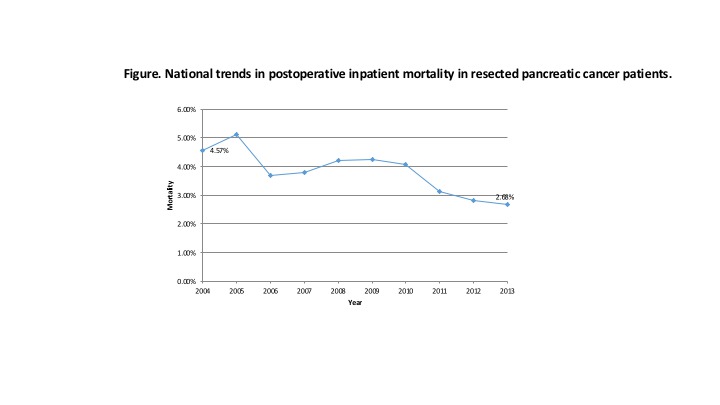
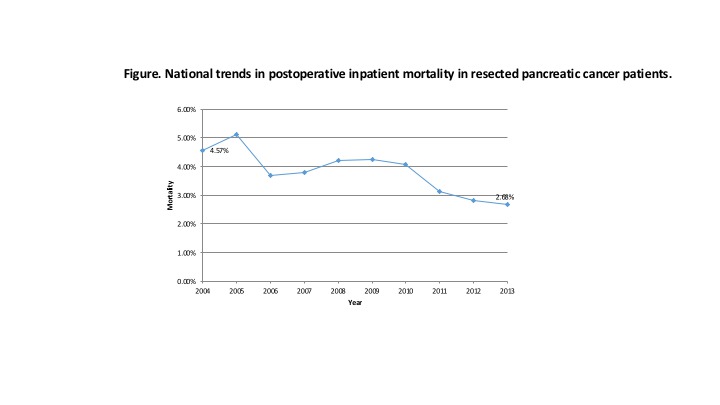
Overall from 2004 to 2013, 13,758 patients underwent resection for pancreatic cancer during their hospitalization. Overall the postoperative inpatient mortality rate was 3.90 (per 100 resected pancreatic cancer hospitalizations). However, during this study period there was 41% overall reduction in mortality from 4.57 in 2004 to 2.68 in 2013 (Figure). After adjusting for demographics and severity of disease, our multivariate analysis demonstrated that reoperation, acute peptic ulcer disease, age above 75, cirrhosis and acute myocardial infarction were the most significant predictors of postoperative inpatient mortality (Table).
Conclusion
Inpatient mortality associated with surgical resection of pancreatic cancer has declined over the past decade. However, risk factors such as reoperation, peptic ulcer disease and older age demonstrate to adversely impact short-term survival in these patients. Future efforts to reduce preventable risk factors may aid in improving postoperative survival.
Table. Significant predictors of postoperative inpatient mortality in resected pancreatic cancer patients
| | Odds ratio | 95% CI | p-value | Age (years)
| | | | | <65 | | Reference | | | 75-84 | 1.87 | 1.30-2.69 | 0.04 | | Co-morbidities | | | | | Reoperation | 5.04 | 3.71-6.84 | <0.05 | | Acute Peptic Ulcer | 4.83 | 1.04-22.32 | <0.05 | | Cirrhosis | 1.76 | 1.12-2.75 | 0.01 | | AMI | 1.73 | 1.10-2.73 | 0.02 | | Electrolyte Disorder | 1.46 | 1.18-1.81 | <0.01 |
Back to 2017 Posters
|