
|
 |
Back to 2017 Posters
PROGNOSTIC IMPACT OF ADDITIONAL PANCREATIC RESECTION FOR CANCER POSITIVE CUT MARGINS DURING DISTAL PANCREATECTOMY FOR PANCREATIC DUCTAL ADENOCARCINOMA
Satoshi Nara*, Minoru Esaki, Yoji Kishi, Toshimitsu Iwasaki, Kazuaki Shimada
Hepatobiliary and Pancreatic Surgery Division, National Cancer Center Hospital, Tokyo, Japan
Background: Invasive cancer at the pancreatic cut margin is sometimes encountered during distal pancreatectomy (DP) for pancreatic cancer. However, the prognostic significance of additional pancreatic resection to achieve a final negative margin has not been well investigated.
Patients and methods: We retrospectively reviewed the records of 181 consecutive patients who underwent DP for pancreatic ductal adenocarcinoma, excluding invasive intraductal papillary mucinous carcinoma, at our hospital from 2001 to 2015. All patients underwent intra-operative frozen section analysis (IOFSA) of the pancreatic stump, with the need for additional pancreatic resection determined by the operating surgeon. Patients who underwent R2 resection, were positive for lavage cytology or para-aortic lymph node metastasis, received preoperative chemotherapy were excluded. Based on the pathologic diagnosis of pancreatic cut margins, patients were divided into five groups: initial margins negative for invasive cancer (Group A); pancreatic margin negative after additional pancreatic resection (Group B); converted to total pancreatectomy due to cancer positive pancreatic margin (Group C); final margins positive for high-grade PanIN (carcinoma in situ) (Group D), and final margins positive for invasive cancer (Group E). The clinicopathological characteristics and prognoses of the five groups were compared, and poor prognostic factors were investigated in all the patients.
Results: IOFSA of the initial pancreatic stump showed that 30 patients harbored invasive cancer, 13 had high-grade PanIN and 10 had low-grade PanIN. Additional pancreatic resection was performed in 37 patients. The pancreatic margin could not be assessed properly in two patients. Groups A, B, C, D and E consisted of 135, 20, 6, 8 and 10 patients, respectively, with median survival times of 58, 44, 49, 33 and 30 months, respectively, and 3-year survival rates of 59%, 61%, 80%, 50% and 27%, respectively (E vs. A; P=0.222, E vs. B; P=0.082, E vs. C; P=0.072, E vs. D; P=0.531, Figure 1). In multivariate analysis, the poor prognostic factors of overall survival were tumor size >3cm, lymph node metastasis (+) and dissected peri-pancreatic tissue margin (+) (P<0.05). In Group E, two patients had recurrence at the pancreatic stump, and both patients died less than 28 months after operation. In Group C, two patients who had no above-mentioned poor prognostic factors, survived more than 46 months without recurrence.
Conclusion: The prognosis of Group E were not significantly different from that of Group C, and the prognostic analysis revealed that postoperative prognosis depended more on the stage of the pancreatic cancer than the pancreatic cut margin status. Therefore, total pancreatectomy to achieve R0 resection should be considered only in selected patients, especially in patients without poor prognostic factors.
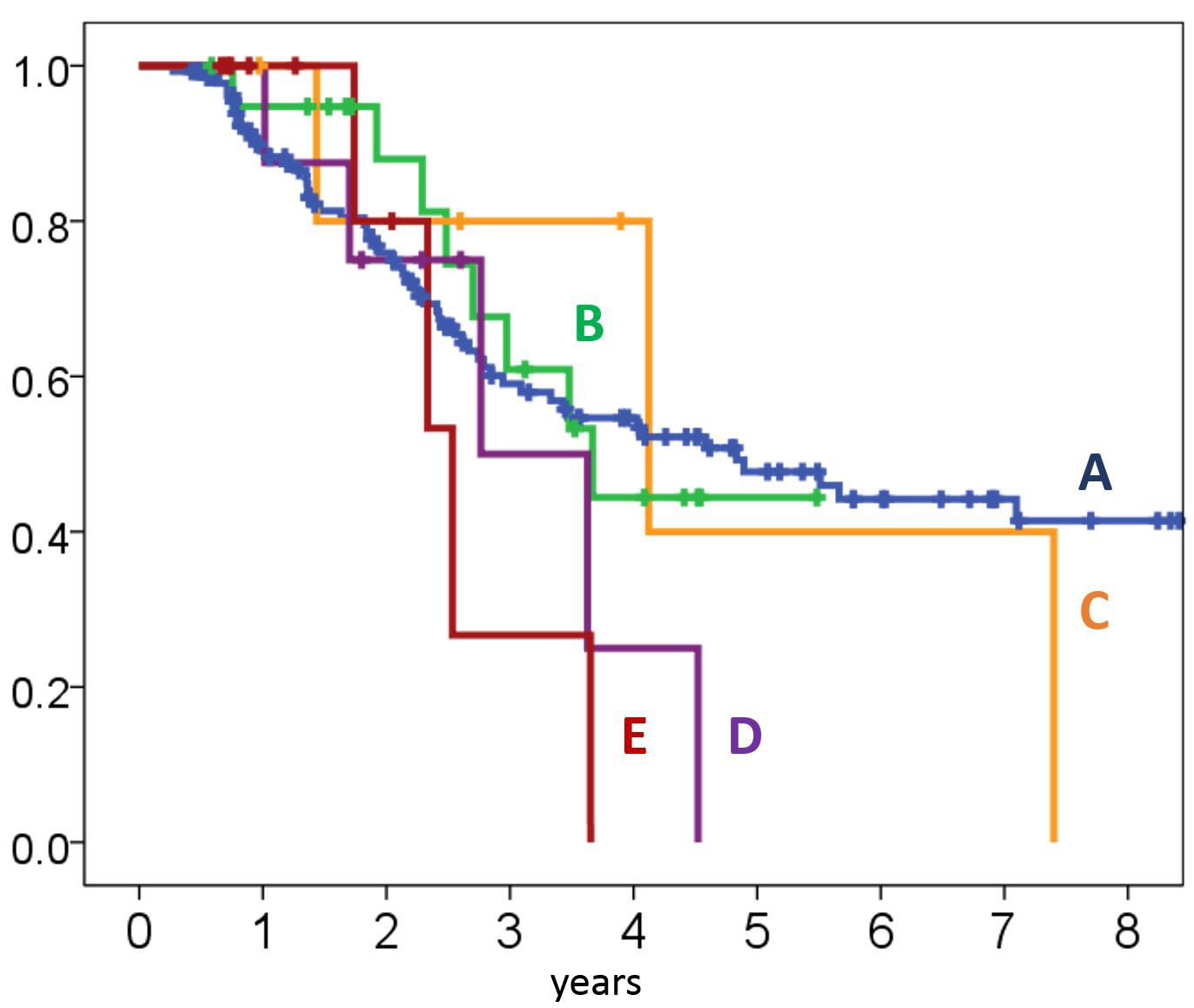
Figure 1 Comparison of overall survival among Group A, B, C, D and E.
Back to 2017 Posters
|

