|
 |
Back to 2017 Posters
ANALYSIS OF FACTORS AFFECTING PATIENT SATISFACTION ONE YEAR AFTER LAPAROSCOPIC FUNDOPLICATION
Herbert M. Hedberg*1,2, Tyler Hall2, JoAnn Carbray2, John G. Linn2,1, Stephen P. Haggerty2,1, Woody Denham2,1, Michael Ujiki2,1
1Surgery, University of Chicago, Chicago, IL; 2Surgery, NorthShore University HealthSystems, Evanston, IL
Background
Laparoscopic fundoplication (FP) is regularly performed for medically refractory GERD or symptomatic hiatal hernia. A well selected and constructed FP is tight enough to prevent gastroesophageal reflux, yet loose enough to allow belching and avoid dysphagia. Bloating and flatulence is a well known side effect of fundoplication, and is seen more commonly with full FPs than with partial FPs. However, factors contributing to overall patient satisfaction after FP have not been investigated. This study sought to correlate overall postoperative satisfaction after FP with preop, intraop and postop factors.
Methods
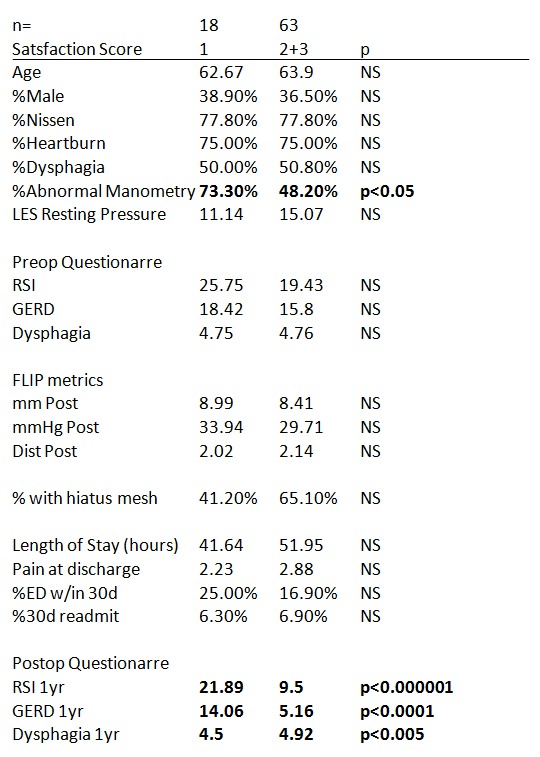
A retrospective review of a prospectively collected database was performed. Queried patients underwent full or partial FP during the years 2009-2015 for GERD and/or symptomatic hiatal hernia. Patients completed validated symptom based and quality of life surveys (Reflux Severity Index, GERD-HRQL, Dysphagia Score, SF36) preop and at one year postop. The patient sample was divided based upon a satisfaction score from 1 to 3 (1=dissatisfied, 2=neutral, 3=satisfied). Individuals with a score of 1 were compared to those answered 2 or 3. Student’s t-test or difference in sample proportion was used to identify significantly divergent preop characteristics, intraop functional luminal imaging probe measurements, and postop symptoms between the two groups.
Results
Eighty-one patients were included in the analysis. 22% of individuals reported a satisfaction score of 1, 32% a score of 2, and 46% a score of 3. Postop symptomatology questionnaires were significantly different between groups 1 vs 2 or 3. Satisfaction of the groups correlated with severity of symptoms as reported in the questionnaires. The only significantly divergent factor identified preop or intraop was the proportion of individuals with abnormal preop manometry, as defined by abnormal peristaltic function or decreased resting lower esophageal sphincter tone (see Table 1). The specific survey questions regarding postop symptoms were compared between groups, and revealed greatest divergence due to questions relating to atypical symptoms of GERD, such as hoarseness, throat clearing, cough, and globus sensation.
Conclusion
In this study of 81 patients receiving FP for GERD and/or symptomatic hiatal hernia, self-reported patient satisfaction one year postop correlated well with validated scales for reflux, GERD and dysphagia symptoms. Greatest divergence between dissatisfied and neutral or satisfied groups occurred with atypical symptoms of GERD. Abnormal preop manometry may be a predictor of dissatisfaction, and may be helpful when selecting appropriate surgical candidates for FP.
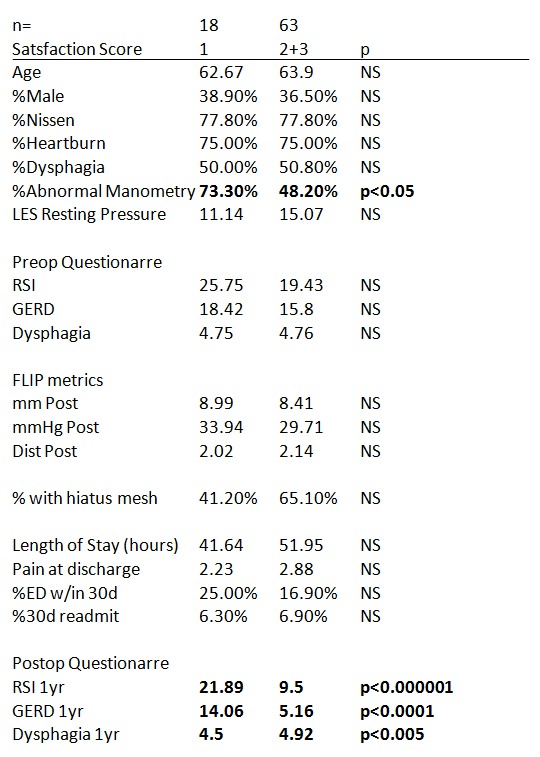
Table 1: Pre, intra, and postop characteristics of satisfied and dissatisfied patient cohorts
Back to 2017 Posters
|