|
Back to 2017 Posters
ENDOSCOPIC NEGATIVE INTRACAVITARY PRESSURE (ENDO-NIP), A CONCEPTUAL MANAGEMENT OPTION FOR GASTRO-CUTANEOUS FISTULA COMPLICATED BY POSTSPENECTOMY BED ABSCESS
Zaheer H. Rizvi*, Alyssa J. Meyer, Navtej S. Buttar
Gastroenterology, Mayo Clinic, Rochester, MN
Background and Aim: Post-surgical complications such as leaks/ fistulas are the source of considerable morbidity and mortality. Success of conservative/radiological interventions is highly variable ranging from 16-46%. Recurrence after surgical repair is not uncommon. Endoscopic interventions are becoming an integral part of therapy for post-surgical complications; however, they are primarily driven by what the devices and accessories can offer. Our aim was to develop strategies that maximize endoscopic negative intracavitary pressure (Endo-NIP) to manage leaks and fistulas in cases where conventional management either failed or was not feasible.
Methods and Results:
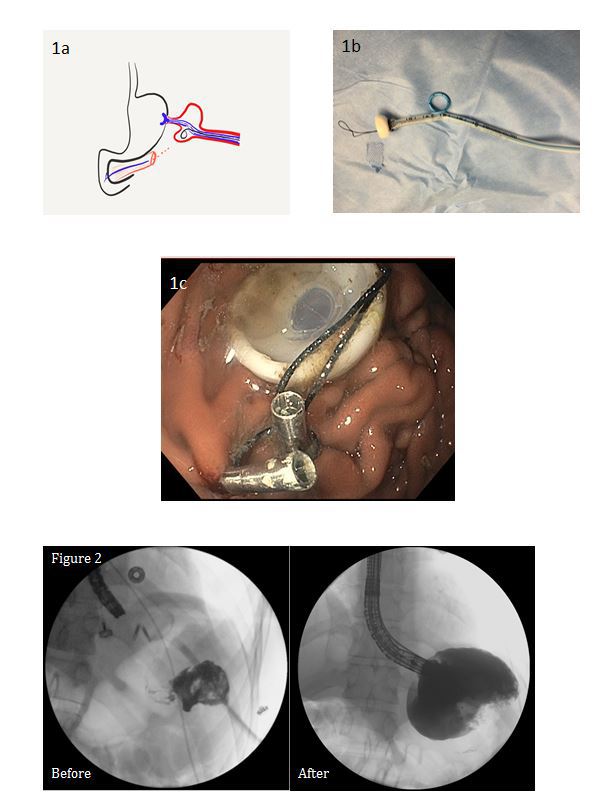
We have used Endo-NIP to manage non-healing leaks/fistulas in mediastinal, peritoneal, retroperitoneal, and pelvic areas. The following example illustrates this concept: a 24-year-old male had non-resolving splenectomy bed abscess communicating with gastric lumen for nearly 5 months after left adrenalectomy, distal pancreatectomy, and splenectomy for adrenocortical carcinoma. A painful transpleural drain was lateralizing gastroduodenal contents without resolution of the cavity (Fig 1a) due to the large fixed and inflamed fistula opening in the stomach. To address these issues we used a novel approach to create a more pronounced NIP. A pediatric endoscope was first introduced via the drain tract into the stomach to measure the distance between gastric mucosal aspect and the cavity, the size of the cavity, and the distance from cavity to skin surface. We refashioned a PEG tube where a silk suture was used to obtrude the opening of the tube towards the bumper side. The PEG tube was marked with the measurements gathered by pediatric scope. At the level where the PEG tube was crossing the abscess cavity, multiple side holes were created in the tube shaft. Through the lumen of the PEG tube shaft, a 12Fr loop drain was brought over a wire that was traversing through one of the holes at the abscess cavity level (Fig 1b). Using a standard PEG placement technique (Fig 1c), the device was placed across the fistula; the loop part of the drain was then carefully deployed into the cavity. Two JP drains were connected, one to the PEG lumen and one to the drain. A complete elimination of this cavity was achieved over an 8 week period. Once the fistula became linear without an obvious cavity, the device was removed and the fistula was closed using a Gore fistula plug and an OverStitch to retain the plug in position. Immediate fluoroscopic exam, as well as subsequent CT, revealed complete closure of the fistula and healing of the skin wound at 90 days follow-up (Fig 2). The patient remains asymptomatic for more than 1 year.
Conclusions: Developing strategies to maximize negative intracavitary pressure by modifying existing devices help expedite the healing of resistant postsurgical leaks and fistulas.
Back to 2017 Posters
|

