|
Back to 2017 Posters
LEFT GASTRIC ARTERY LYMPH NODES SHOULD BE INCLUDED IN D1 LYMPH NODE DISSECTION IN GASTRIC CANCER
Naruhiko Ikoma*, Mariela Blum, Jeannelyn Estrella, Keith Fournier, Paul Mansfield, Jaffer Ajani, Brian Badgwell
Univ. Texas MD Anderson Cancer Center, Houston, TX
Introduction:
Definitions of the extent of D1 and D2 lymph node (LN) dissection have been modified in a Japanese classification of gastric cancer. Recent editions include left gastric artery (#7) LN in the recommended extent of D1 LN dissection, but this recommendation has not been validated by Western institutions, and National Comprehensive Cancer Network guidelines still categorize #7 LNs as a part of the N2 LN group. We sought to investigate the frequency of #7 LNs metastases and the survival impact of #7 LNs metastases in gastric cancer.
Methods:
We reviewed data from a prospectively maintained database of gastric cancer patients who had undergone resection of gastric or gastroesophageal cancer at our institution between 2003 and 2016. Frequencies of #7 LNs metastases were calculated. Univariate and multivariate analyses were conducted to examine risk factors for #7 LNs metastases and the impact of these metastases on overall survival, adjusted by pathological N stage (AJCC Cancer Staging Manual, 7th Edition).
Results:
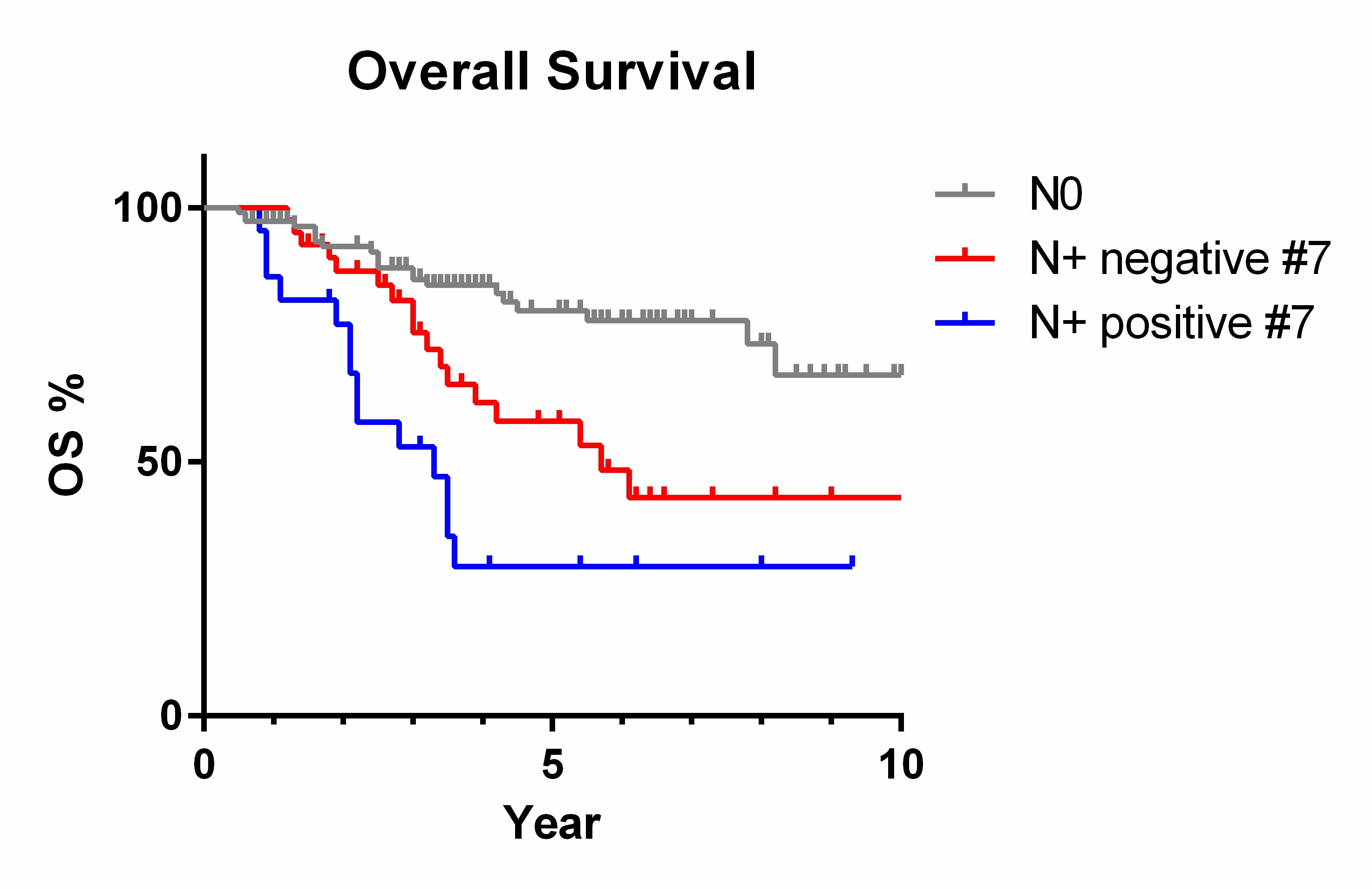
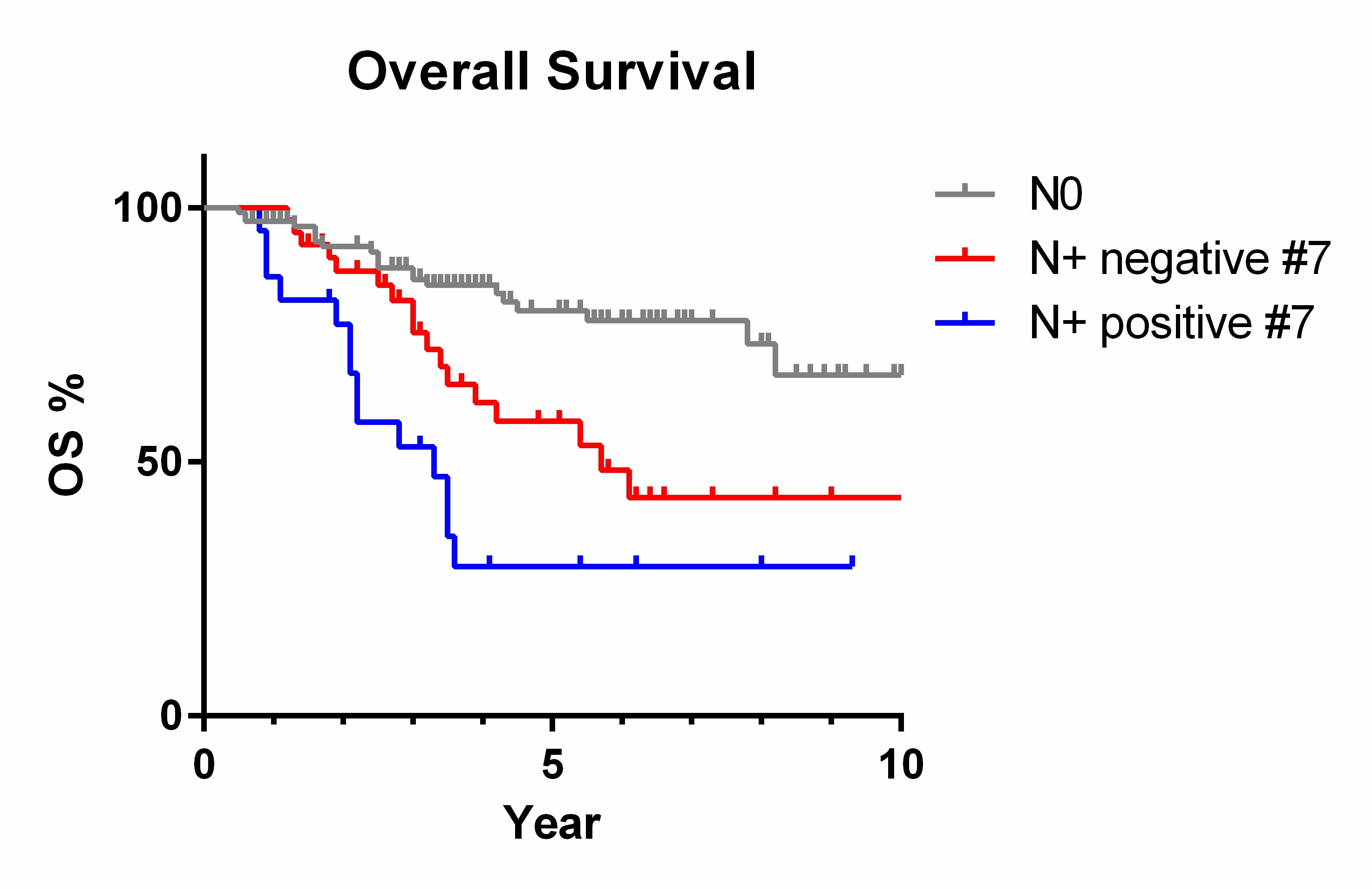
We identified 173 patients who had undergone gastrectomy for gastric or gastroesophageal cancer and had a separate pathologic assessment of #7 LNs. Median age was 64 years, and 56% were male. Of these patients, 114 (66%) were treated with preoperative therapy, most commonly with chemoradiation therapy (47%, 81/173). D1+/D2 LN dissection was performed in the vast majority of patients (97%, 167/173); the median number of LNs examined was 26 (interquartile range, 20-34), and the median number of #7 LNs examined was 5 (interquartile range, 3-8). We identified 22 patients (13%) who had #7 LNs metastases, which accounted for 35% (22/63) of pN-positive patients. No preoperative factors (including age, gender, resection year, preoperative therapy, tumor location, histologic grade, signet-ring cell, or pretreatment EUS T and N stages) were significantly associated with #7 LNs metastases by univariate or multivariate analysis, although a trend was observed with type of procedure; patients with #7 LNs metastases underwent total gastrectomy more frequently (59%, 13/22) than did those without (36%, 54/151; odds ratio 0.42, 95% confidence interval 0.17-1.05; p=0.063). Patients with #7 metastases had shorter overall survival (Fig. 1) compared with other pN-positive patients (hazard ratio 2.00, 95% confidence interval 1.02-4.78; p=0.048). However, this association did not remain significant after adjustment by pN stage (hazard ratio 1.53, 95% confidence interval 0.68-3.43; p=0.306).
Conclusion:
#7 LNs metastases were common in gastric cancer, but their survival impact was not significant after adjustment by pN stage. No preoperative factors were helpful in identifying patients with #7 LNs metastases. #7 LNs should be routinely dissected in gastric cancer patients.
Back to 2017 Posters
|