|
Back to 2017 Posters
HOW MUCH DOES HOSPITAL VOLUME ACCOUNT FOR QUALITY AFTER MAJOR HEPATECTOMY?
Yanik J. Bababekov*, Zhi Ven Fong, Daniel A. Hashimoto, Sahael M. Stapleton, David W. Rattner, Keith D. Lillemoe, David C. Chang
Surgery, Massachusetts General Hospital, Boston, MA
Background: Hospital-volume (HV) is an important predictor of patient outcomes in surgery. However, the relative contribution of HV, hospital structural factors (HSF), and patient factors (PF) in predicting post-operative outcomes is unknown.
Methods: The National Inpatient Sample (NIS) database was linked with the American Hospital Association (AHA) database to study patients ≥ 18 years undergoing major hepatectomy from 1998-2011. The relative contribution of and overlap between three groups of variables (HV, HSF, and PF) to inpatient mortality was determined based on McFadden’s pseudo-R2 from multivariate logistic regression models. A model with higher pseudo-R2 explains more observed variation in the outcome. Model performances were assessed using c-statistics. A model with a higher c-statistic is better at discriminating patients who may have two different possible outcomes.
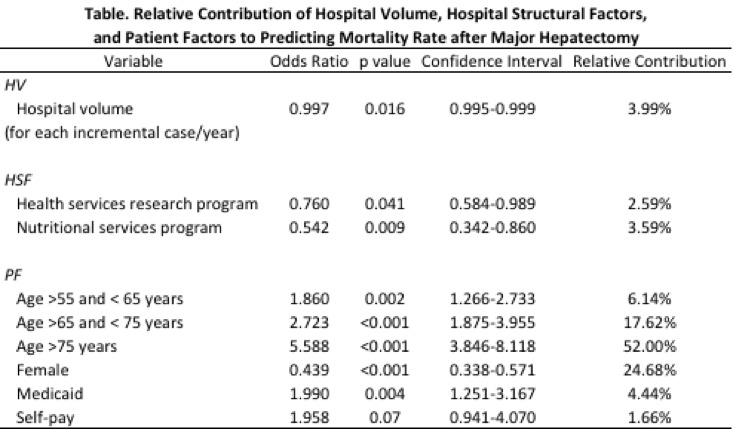
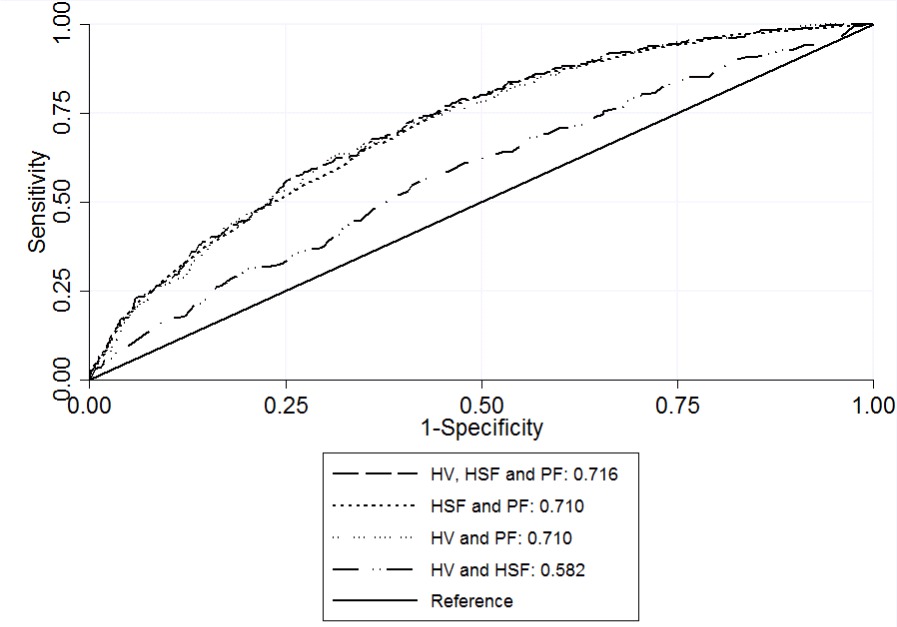
Results: A total of 12,693 patients underwent hepatectomy at 721 hospitals. The overall inpatient mortality rate was 2.2%. Independent predictors of mortality included HV; HSF, including health services research program and nutrition program; and PF, including gender and age >55 years. The pseudo-R2 for the inpatient mortality model was 0.064; among which, HV accounted for 3.9%, HSF for 14.6%, and PF for 85.6% of the explained variation (Table). A model with HV and HSF (c-statistic 0.582, p <0.05) only marginally improved performance beyond the reference, or chance alone. However, adding PF significantly improved the performance of all models (c-statistics 0.710-0.716, p <0.05, Figure).
Conclusion: While hospital volume predicts inpatient mortality in patients undergoing major hepatectomy, its relative contribution to quality is less than that of hospital structural factors and patient factors. Patient factors account for most of the explained variation in mortality rates. Policy decisions should not be anchored solely on hospital volume given its small relative contribution to quality. A quality improvement approach should be aimed at optimizing care by identifying modifiable factors in addition to hospital volume.
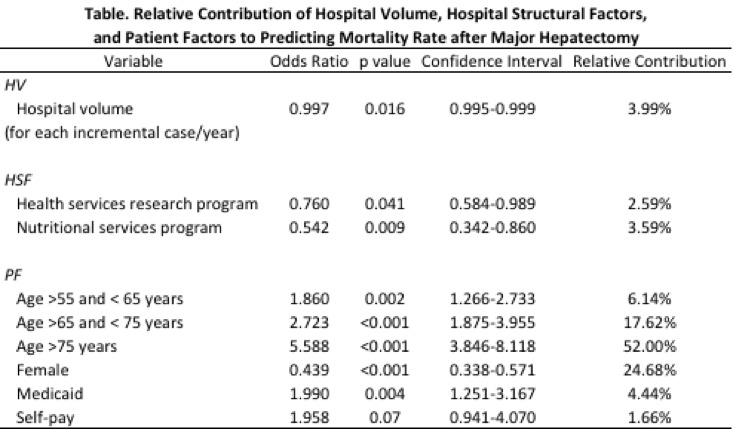
HV, hospital volume; HSF, hospital structural factors; PF, patient factors
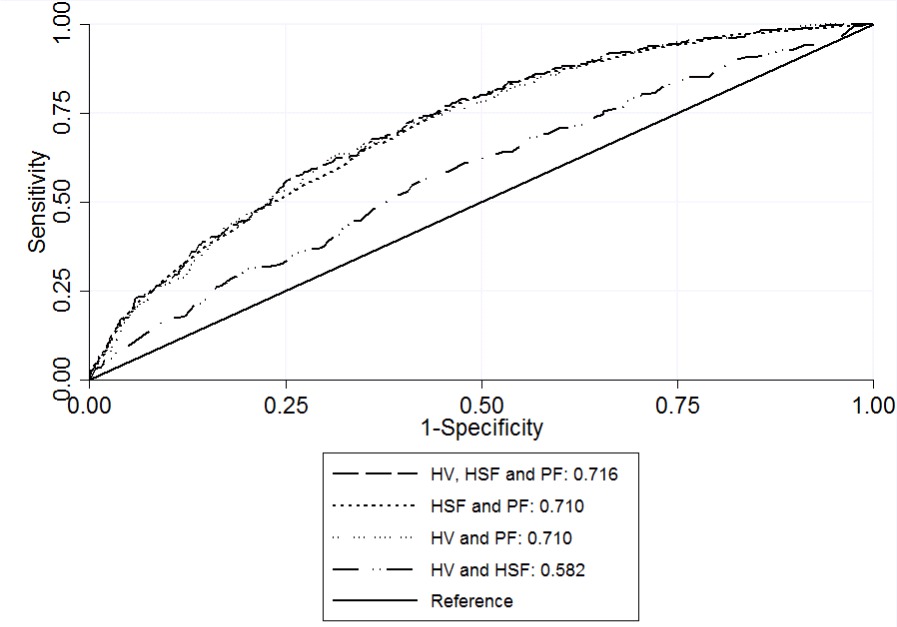
Figure. Predictive performance (c-statistics) of full model and models with and without HV, HSF, and PF.
HV, hospital volume; HSF, hospital structure factors; PF, patient factors.
Back to 2017 Posters
|