
|
 |
Back to 2017 Posters
FOR PATIENTS WITH HEPATOCELLULAR CARCINOMA, PERIOPERATIVE TRANSFUSION IS A CO-VARIATE FOR SHORT-TERM MORBIDITY AND MORTALITY BUT DOES NOT IMPACT LONG-TERM ONCOLOGIC OUTCOMES
Bradford Kim*, Jason Denbo, Catherine Davis, Yun Shin Chun, Jean Nicolas Vauthey, Ching-Wei Tzeng, Thomas Aloia
Surgical Oncology, University of Texas MD Anderson Cancer Center, Houston, TX
Background: The purpose of this project was to determine the relationship between perioperative blood transfusion and outcomes after hepatectomy for hepatocellular carcinoma (HCC).
Methods: Query of the institution’s prospectively maintained hepatobiliary tumor database identified 161 patients treated with hepatectomy for hepatocellular carcinoma between 2003 and 2013. Patient and operative characteristics were compared between patients who received packed red blood cell transfusion (T) versus those who had no transfusions (NT) during the perioperative period. To differentiate surgical, liver-related and cancer-related survivals, patients who died within 90 days of surgery were excluded from long-term survival analysis. Standard statistical methods were utilized.
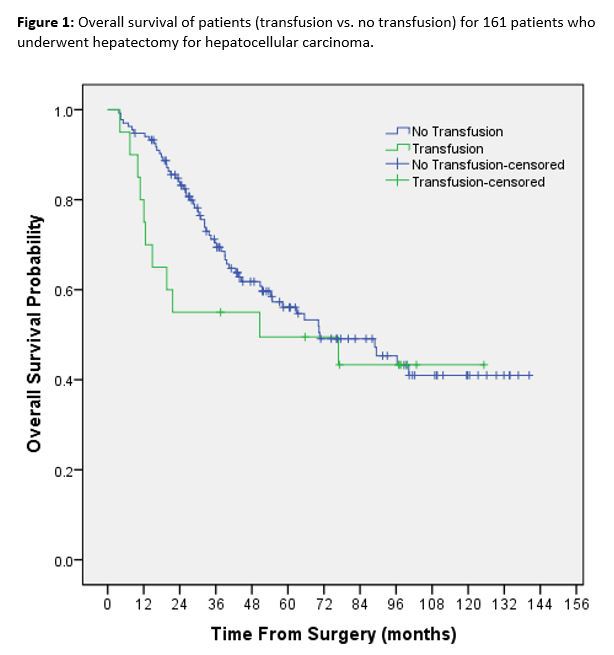
Results: Throughout the study period a uniform set of criteria was used for transfusion based on hemodynamic parameters, and not on laboratory thresholds. Median age was 63.1 years (range: 2.7-88.8), 61.5% were male, and 78.3% had an ASA ≥3. Presence of cirrhosis (28.7% vs. 20%, p=0.468), median tumor number (1 vs. 1, p=0.993), median tumor size (50 mm vs. 76.5 mm, p=0.059), number of major liver resections performed (54.4% vs. 64%, p=0.375), and length of operation (210 minutes vs. 252.5 minutes,p=0.16) were similar between NT and T, respectively. Twenty-five patients (15.5%) received a perioperative transfusion. In patients who received transfusions preoperative hemoglobin was lower (median 13.4 mg/dL [IQR 10.9-12.9] vs. 12.1 mg/dL [IQR 10.9-12.9], p<0.001), while no difference in preoperative platelet counts was observed (median 220 mg/dL[IQR 163.3-281.5] vs. 236 mg/dL[IQR 169.5-316], p=0.366). Compared to NT patients, T patients had a greater median estimated blood loss (EBL) (200 mL vs. 700 mL, p<0.001), median length of stay (LOS) (6 days[IQR 5-8] vs. 8 days[IQR 6-19.5], p=0.001), surgical complication rate (28.7 vs. 68%, p<0.001), major complication rate (8.1% vs. 40%, p<0.001), and 90-day mortality rate (1.5% vs. 20%, p=0.002). Outcomes analysis determined that EBL>250 mL, ‘two surgeon’ technique, transfusion, major liver resection, and tumor size>50 mm were associated with liver-related complications (all p<0.05). Factors associated with 90-day mortality included hypertension, any surgical complication, major complications, bile leak, liver failure, LOS>6 days, and transfusion (all p<0.05). In contrast, at a median follow up of 39.7 months, overall 5-year survival was similar between NT and T patients on multivariate analysis (56.1% vs. 49.5%, OR=1.1, p=0.747),[Figure 1].
Conclusion: These data suggest that perioperative transfusion in patients with HCC is a co-variate for short-term liver-related complications along with increased blood loss and magnitude of hepatectomy. After the postoperative period, however, transfusions do not independently act to reduce long-term HCC survivals.
Back to 2017 Posters
|

