|
Back to 2017 Posters
VASCULOBILIARY ANATOMY IN THE UMBILICAL FISSURE: EVALUATION BY TWO-DIMENSIONAL AND THREE-DIMENSIONAL IMAGING
Guwei Ji*
Department of liver surgery, First Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu, China
Background Thoroughly understanding the two-dimensional (2D) and three-dimensional (3D) radiologic features of vasculobiliary anatomy in the umbilical fissure (U-point) is pivotal for preoperative evaluation and surgical management of hilar cholangiocarcinoma (HC).
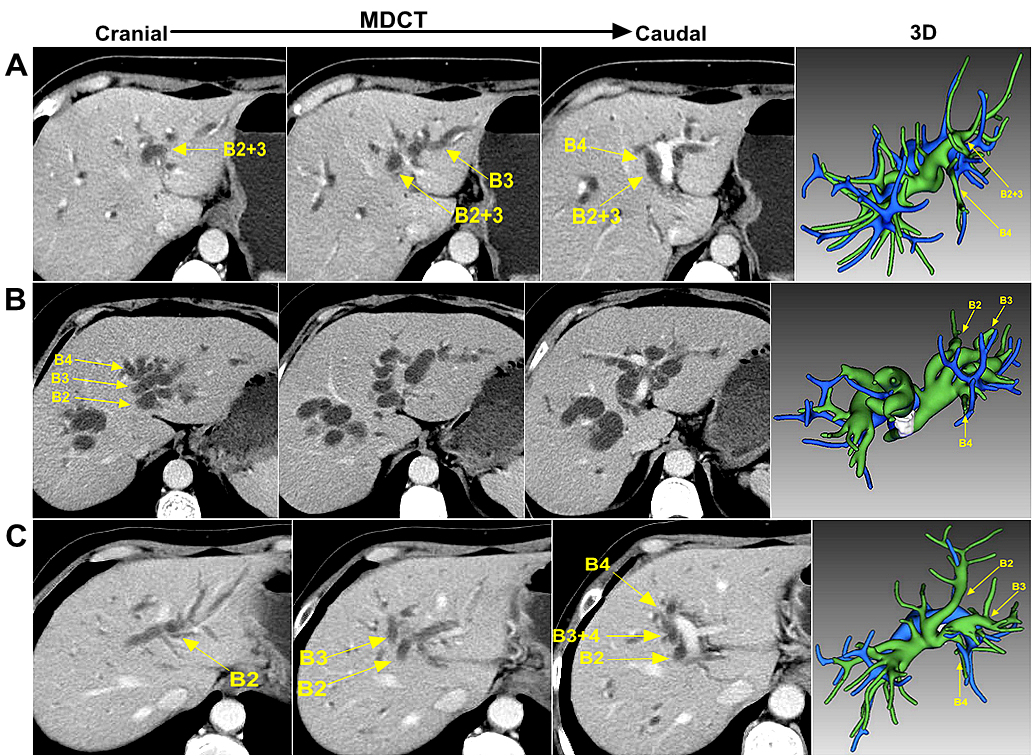
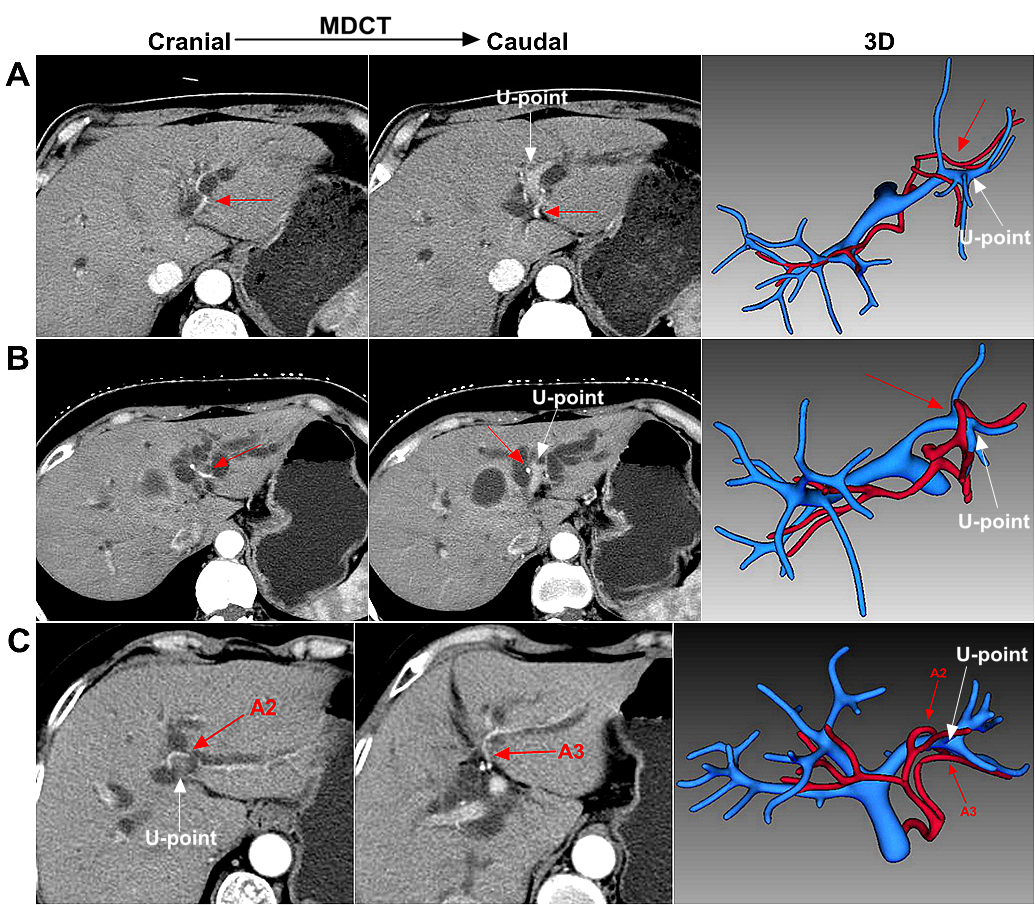
Methods A retrospective study of 159 patients with Bismuth type I, II and IIIa HC, who received surgery at our institution from November 2012 to September 2016, was conducted. Anatomic structures were evaluated using multi-detector computed tomography (MDCT) and 3D visualization system by one hepatobiliary surgeon and radiologist independently and respectively. Normal confluence pattern of left biliary system was defined as the left medial segmental bile duct (B4) joining the common trunk of segment II (B2) and segment III (B3) ducts while aberrant confluence patterns were classified into three types: type I, triple confluence of B2, B3, and B4; type II, B2 draining into the common trunk of B3 and B4; type III, other patterns. Surgical anatomy of B4 was classified into the central, peripheral and combined type based on its relation to the hilar confluence. The lengths from the bile duct branch of Spiegel’s lobe (B1l) to the orifice of B4 and the junction of B2 and B3 were measured on 3D images. The anatomy of left hepatic artery (LHA) was classified based on different origins and the spatial relationship related to the U-point.
Results Normal confluence pattern of left biliary system was observed in 71.1% of all patients and aberrant patterns were type I in 11.9%, type II in 12.6% and type III in 4.4%. The length from B1l to the junction of B2 and B3 was 12.1 ± 3.1mm in type I, which was significantly shorter than that in normal configuration (30.0 ± 6.8mm, p<0.001) but significantly longer than that in type II (9.6 ± 3.4mm, p= 0.019). Surgical anatomy of B4: peripheral type was most commonly seen (74.2%), followed by central type (15.7%) and combined type (10.1%). The distance between B1l and B4 was 8.4 ± 2.4mm in central and combined type , which was significantly shorter than that in peripheral type (14.5 ± 4.1mm, p<0.001). A replaced or accessory LHA from the left gastric artery was present in 6 (3.8%) and 9 (5.7%) patients, respectively. LHA running along the left-caudal position of U-point was present in 143 cases (89.9%), along the right-cranial position of U-point in 9 cases (5.7 %), and combined position in 7 cases (4.4%). Interobserver agreement of two imaging modalities was almost perfect in biliary confluence pattern (kappa = 0.90), substantial in surgical anatomy of B4 (kappa = 0.74), and perfect in LHA (kappa = 1.00).
Conclusions Accurate evaluation of surgical anatomy in the U-point can be accomplished by successive review of 2D images but 3D visualization and simulation allows detailed hepatic anatomy and individualized surgical planning for sophisticated and advanced HC.
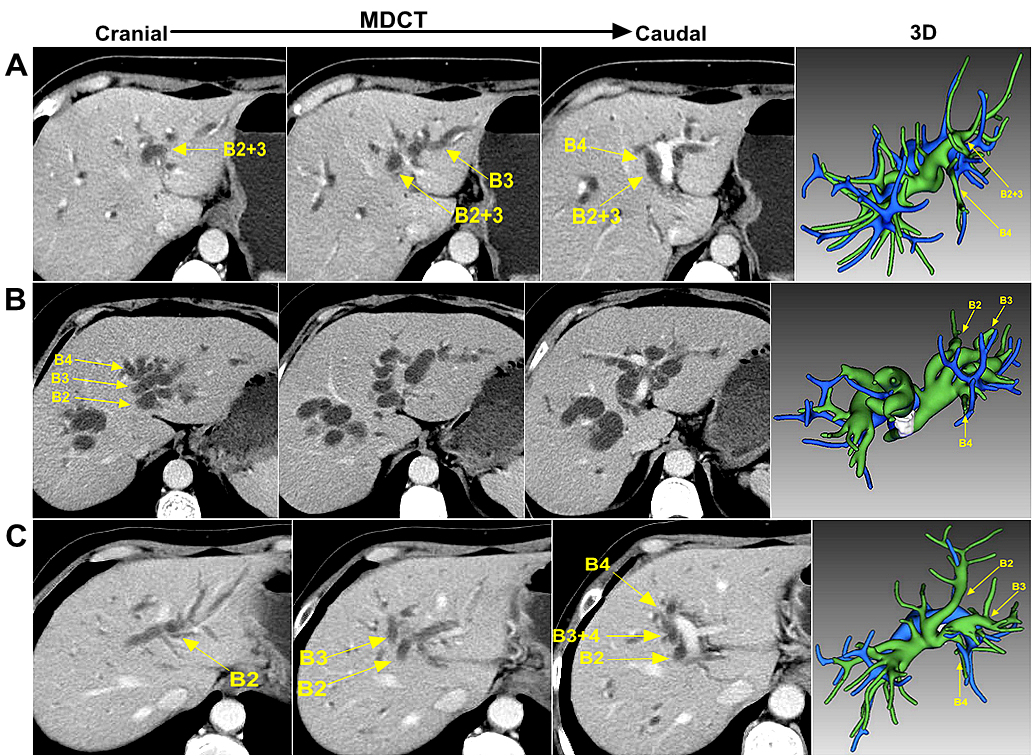
Fig.1 Classification of the confluence pattern of left biliary system according to transverse MDCT images and 3D reconstruction model (A) Normal configuration, B4 joining the common trunk of B2 and B3; (B) type I variation, triple confluence of B2, B3, and B4; (C) type II variation, B2 draining into the common trunk of B3 and B4
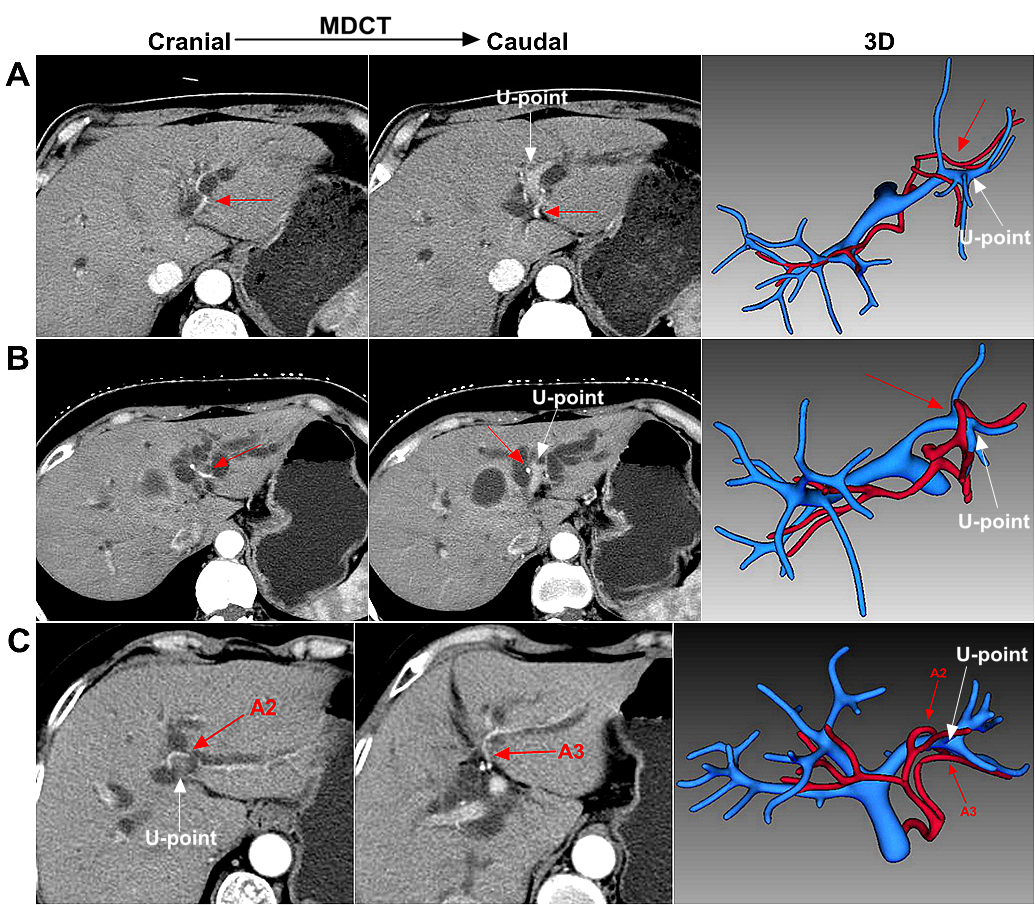
Fig.2 Classification of the spatial relationship between the LHA (red arrow) and the U-point according to transverse MDCT images and 3D reconstruction model (A) L type, LHA running along the left-caudal position of the U-point; (B) R type, LHA running along the right-cranial position of the U-point; (C) Combined type, one segmental branch of the LHA running along the right-cranial position of the U-point, and the other from the left-caudal position of the U-point.
Back to 2017 Posters
|