|
Back to 2017 Posters
LONG-TERM SURVIVAL AMONG MISMATCH REPAIR DEFICIENT CHOLANGIOCARCINOMAS ASSOCIATED WITH LYNCH SYNDROME
Jordan M. Cloyd*, Yun Shin Chun, Jason Denbo, Milind Javle, Rachna Shroff, Jean Nicolas Vauthey, Thomas Aloia, Amanda Cuddy, Miguel A. Rodriguez-Bigas, Y. Nancy You
Surgical Oncology, MD Anderson Cancer Center, Houston, TX
Introduction: Patients with Lynch syndrome (LS) have a significantly elevated lifetime risk of developing bile duct cancers compared to the general population. However, few studies have characterized the clinical characteristics, genetic features or long-term outcomes of mismatch-repair (MMR) deficient cholangiocarcinomas associated with LS.
Methods: A retrospective review of our prospectively maintained Genetic Counseling and Familial High Risk GI Cancer Clinic databases identified all patients with biliary tract adenocarcinomas evaluated from 2006-2016. Patients whose tumors showed evidence of MMR deficiency by immunohistochemistry and/or who carry germline mutations in MLH1, MSH2, MSH6 or PMS2 were included.
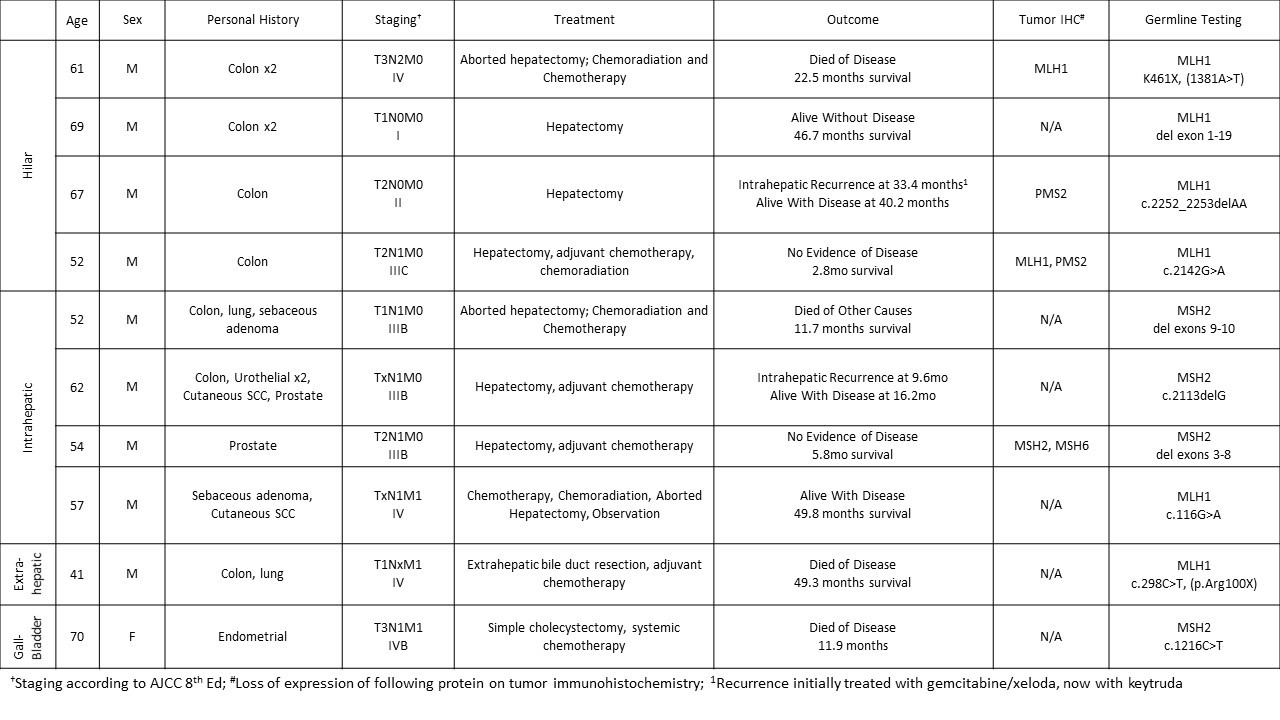
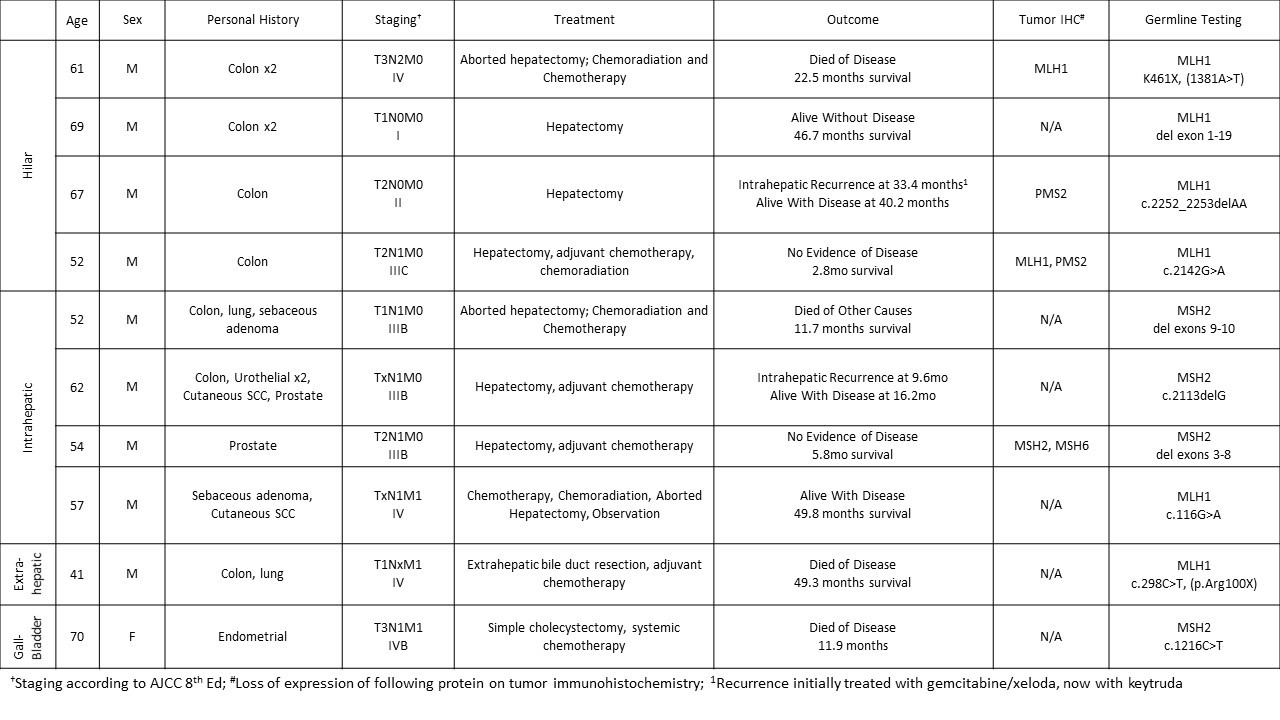
Results: Ten patients with cholangiocarcinomas were identified: 4 hilar, 4 intrahepatic, 1 extrahepatic, and 1 gallbladder cancer (Table). Nine were male and the median age at diagnosis was 59 (range 41-70). Germline mutations were found in MLH1 (6 patients) and in MSH2 (4 patients). All had a personal history of a LS-associated malignancy, most commonly (70%) colorectal cancer. The majority (80%) presented with either regional nodal or distant metastatic disease. Nine (90%) were surgically explored, and margin negative resection was possible in six. Chemotherapy (90%) and/or chemoradiation (40%) was administered to most patients. Among the 5 patients presenting with non-metastatic disease who underwent surgical resection with curative intent, the median overall and recurrence free survival rates were 49.3 and 33.4 months, respectively. The median overall survival (OS) for the 5 patients not treated with curative intent was 17.2 months. Patients with MSH2 mutations had worse OS compared to those with MLH1 mutations (11.9 vs 49.3 months, p=0.04).
Conclusions: MMR deficient cholangiocarcinomas associated with LS are rare and present predominantly in men after the 4th decade at advanced stages. Our case series suggests that long term outcomes may be more favorable than contemporaneous cohorts of non-Lynch associated cholangiocarcinomas. Given the emerging promise of immunotherapy for patients with MMR deficient malignancies and the high proportion of patients with underlying germline mutations, tumor testing for MMR deficiency followed by confirmatory germline testing should be considered in patients with cholangiocarcinoma and a personal history of other Lynch-associated cancers.
Back to 2017 Posters
|