|
 |
Back to 2017 Posters
CLINICAL OUTCOMES AND RESEARCH UTILIZATION FOR THE WHIPPLE PROCEDURE: A 10-YEAR NATIONWIDE ANALYSIS
Paul T. Kroner*2, Pichamol Jirapinyo1, Marwan S. Abougergi3, Thomas Clancy1, Christopher C. Thompson1
1Brigham & Women's Hospital, Boston, MA; 2Mt. Sinai St. Luke's / Mt. Sinai West, New York, NY; 3johns hopkins bayview medical center, Baltimore, MD
Background
Whipple’s procedure (WP) is known to entail significant mortality risk, morbidity and high economic impact. Recent studies show decreasing mortality rates in WP, though morbidity rates remain elevated. Although some studies have evaluated perioperative morbidity and mortality at a national level, these studies are now relatively old with a limited number of outcomes. The aim of this study was to explore the changes in procedure use, postoperative early morbidity and mortality, and resource utilization in patients that underwent Whipple procedure throughout the past decade using a national database.
Methods
Retrospective cohort study using the National Inpatient Sample from 2004 to 2013. All patients with an ICD-9CM code for any procedural code of Whipple procedure were included in the study. No patients were excluded. The primary outcome was inpatient mortality, stratifying by hospital teaching status. Secondary outcomes were morbidity, measured by development of postoperative cardiac arrest, thromboembolic events, infection, respiratory compromise, shock, bleeding, and fistula; resource utilization, measured by length of hospital stay (LOS), hospitalization charges and costs (adjusted for inflation). Odds ratios and means were adjusted for age, sex, race, income in the patient’s zip code, Charlson Comorbidity Index, hospital region, rural location, size and teaching status with multivariate logistic regression.
Results
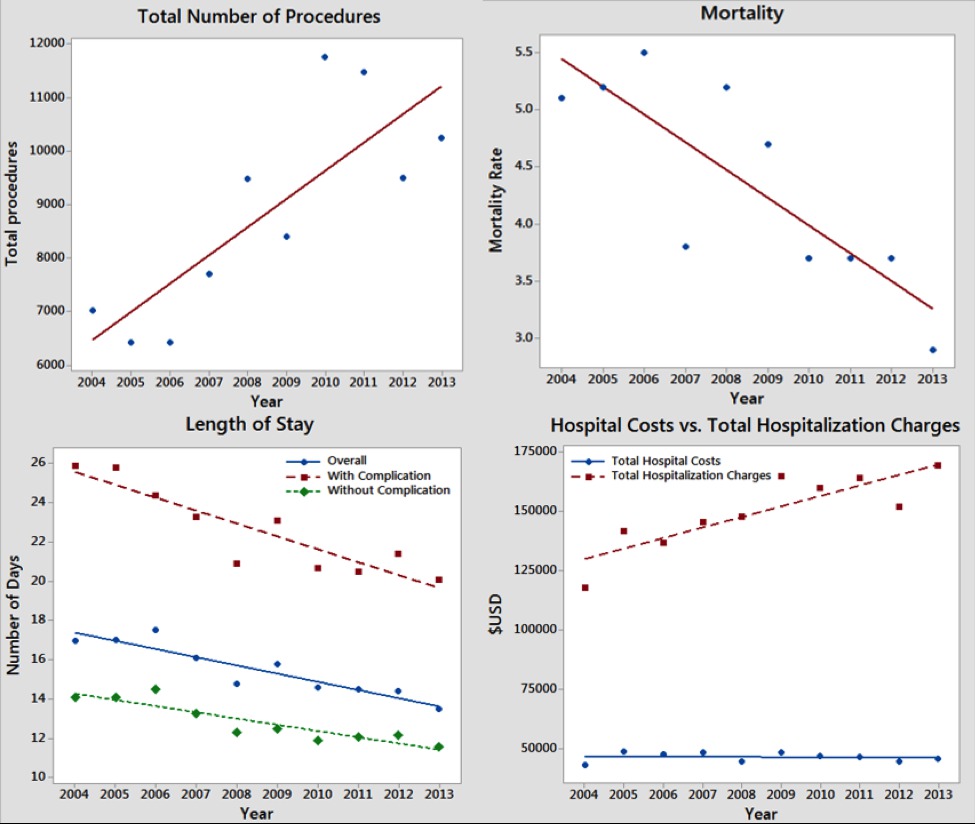
84,062 patients who underwent Whipple procedure were included in the study. Mean age was 64 years and 48% were female. All values for the primary outcome are shown in Table 1. The number of Whipple procedures increased by 30% in the past decade. Crude mortality decreased 38%, from 4.27% to 2.63% (p<0.01). Mortality at teaching institutions decreased from 3.5% to 2.3% (p<0.01), while mortality at non-teaching institutions decreased from 6.8% to 4.8% (p<0.01). Post-operative complication rates are shown in Table 1. LOS decreased by 20% from 16.3 to 13.1 days (p<0.01). Total hospitalization charges increased in 27%, from $117,423 to $149,258 (p<0.01), while total hospital costs remained virtually unchanged from $45,461 to $45,264 (p=0.25).
Conclusion
Despite having peaked in the early half of the past decade, mortality rates for the Whipple procedure decreased significantly in the latter half of the study. This is likely due to many factors, including broader adoption of the laparoscopic procedure, increasing number of yearly performed procedures and increased surgeon experience. Despite the improvement in mortality rates morbidity rates have increased, specifically the incidence of thromboembolic disorders and post-operative shock. Regarding resource utilization, hospital length of stay has decreased and hospital costs have remained unchanged, however, total charges have increased.
Table 1 - Crude and adjusted values for Mortality, Length of Stay, Total Hospitalization Charges and Hospital costs in patients who underwent Whipple’s procedure in 2013 compared to 2004 and evolving post-operative complications in patients with Whipple’s
| 2013 vs. 2004 | Adjusted OR/Mean (95%CI) | p-value | | Mortality | 0.53 (0.34 - 0.82) | <0.01 | | Length of Stay | -3.1 days (-4.8 - -1.4) | <0.01 | | Total Hosp. Charges | $5,001 ($2,773 - $7,229) | <0.01 | | Total Hosp. Costs | $12 (-$573 - $597) | 0.97 | | | Percent Change | Value Change | p-value | | Overall Mortality | -38% | 4.3% - 2.6% | <0.01 | | Teaching Hospital | -34% | 3.5% - 2.3% | <0.01 | | Non-Teaching Hospital | -29% | 6.8% - 4.8% | <0.01 | | Length of Stay | -20% | 16.3 - 13.1 days | <0.01 | | With Complication | -22% | 25.9 - 20.1 days | <0.01 | | Without Complication | -18% | 14.1 - 11.6 days | <0.01 | | Total Hosp. Charges | +27% | $117,423 - $149,258 | <0.01 | | Total Hosp. Costs | -1.8% | $45,461 - $45,264 | 0.25 | | Post-Operative Complication | Incidence in 2004 vs 2013 | 95% Confidence Interval | p-value | | Deep venous thrombosis | 1.02 - 3.18% | 1.10 - 1.19 | <0.01 | | Pulmonary Embolism | 0.88 - 1.96% | 1.08 - 1.19 | <0.01 | | Portal Vein Thrombosis | 0.24 - 0.56% | 1.02 - 1.20 | 0.02 | | Infection | 7.77 - 8.27% | 0.99 - 1.05 | 0.10 | | Pulmonary Compromise | 10.3 - 5.39% | 0.91 - 0.96 | <0.01 | | Shock | 0.51 - 1.79% | 1.02 - 1.16 | 0.01 | | Bleeding | 5.03 - 5.31% | 0.96 - 1.02 | 0.56 | | Fistula Development | 1.49 - 1.01% | 0.92 - 1.03 | 0.30 | | Cardiac Arrest | 3.40 - 2.63% | 0.93 - 1.01 | 0.09 |
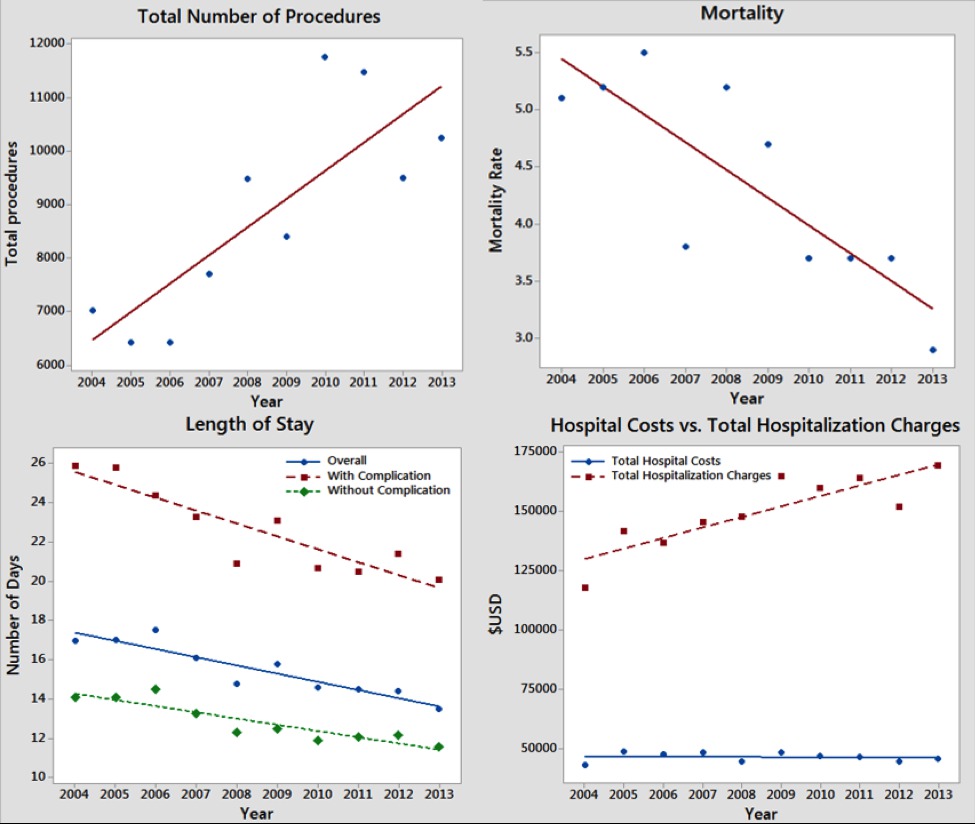 Figure 1 - Total number of cases, mortality, length of stay, total hospitalization charges and total hospital costs trends during the past decade for patients undergoing Whipple procedure in the United States.
Back to 2017 Posters
|