|
Back to 2017 Posters
ADJACENCY OF RURAL COUNTY OF RESIDENCE TO AN URBAN COUNTY MAY DETERMINE SURVIVAL FOR STAGE I PANCREATIC CANCER
Amir A. Khan*, Emily C. Sturm, Erin Mackinney, Elaine J. Buckley, Benjamin Rejowski, John D. Mellinger, Sabha Ganai
Department of Surgery, Southern Illinois University, Springfield, IL
Background: While pancreatic surgery has become increasingly centralized, the impact of rural location on overall survival has not been studied for pancreas cancer. We hypothesized that in patients with Stage I pancreatic cancer, rural patients would have decreased rate of pancreatectomy and a survival disadvantage compared to urban patients.
Methods: A retrospective analysis of the Surveillance, Epidemiology, and End Results Program (SEER) database was performed reviewing patients with Stage I pancreatic cancer from 2004-2013. Patients were examined based on Rural-Urban Continuum Code (RUCC), with county of residence classified as urban, rural adjacent to urban, and rural non-adjacent to urban. The primary outcome measured was the rate of surgical resection. Multivariate logistic regression and Cox proportional hazard models were used to examine likelihood of undergoing pancreatectomy and independent predictors of survival, respectively.
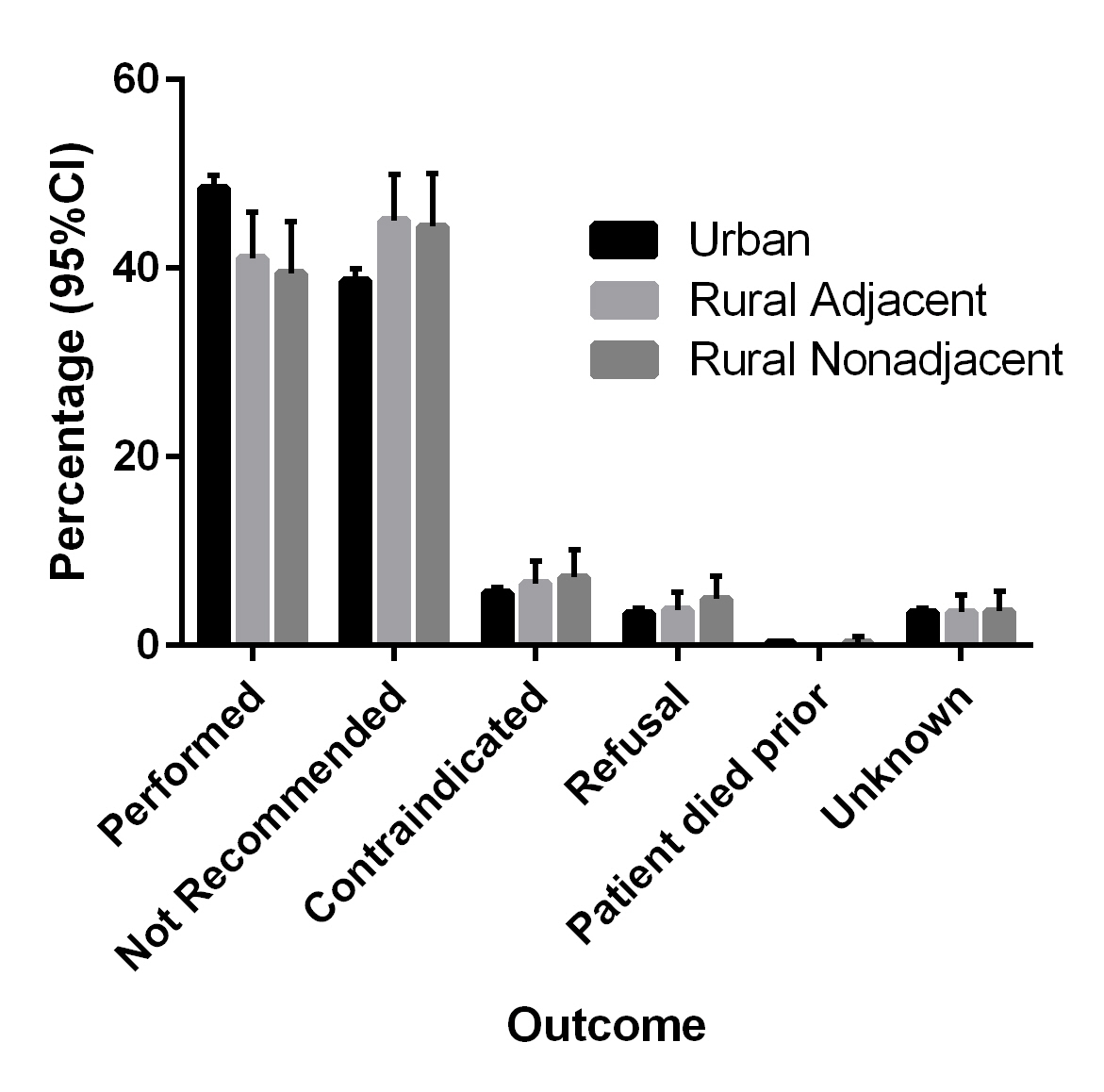
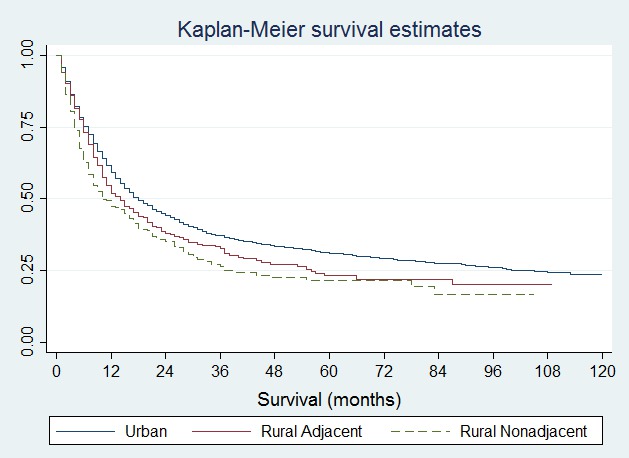
Results: Of 80,130 patients with pancreatic cancer, 6,196 were Stage I pancreatic cancer; 6,192 of these had an available RUCC code, and 2947 underwent pancreatectomy. Resection was performed on 48.5% of patients residing in urban counties compared to 41.1% and 39.5% of patients residing in rural-adjacent and rural non-adjacent counties, respectively, with increased rates of surgery not being recommended in rural counties (Figure 1; p=0.002). Multivariate logistic regression controlling for demographics and time period of diagnosis revealed a lower likelihood of undergoing pancreatectomy among patients from rural counties with an adjusted odd ratio 0.69 (95% CI; 0.53-0.90) and 0.68 (95% CI; 0.51-0.91) for adjacent and non-adjacent cohorts. For all patients, regardless of resection status, median survival of 18 months was seen for urban patients, 14 months for rural-adjacent patients, and 10 months for non-adjacent patients with Stage I pancreas cancer (Figure 2; p<0.001). Controlling for demographics, time period of diagnosis, receipt of surgery, and radiation therapy, while there was no difference between survival within rural-adjacent and urban counties (HR 1.07; 95% CI, 0.93-1.22), patients residing in rural non-adjacent counties had a statistically significant decrease in survival (HR 1.28; 95% CI, 1.10-1.48; p <0.001) compared to urban counties.
Conclusions: As we hypothesized, patients residing in both rural adjacent and rural non-adjacent counties were significantly less likely to undergo pancreatectomy than patients in urban counties, but there was a survival disadvantage only for rural non-adjacent patients. Further exploration of rural disparities and implications of driving distance, referral barriers, and access to health care for pancreas cancer is warranted.
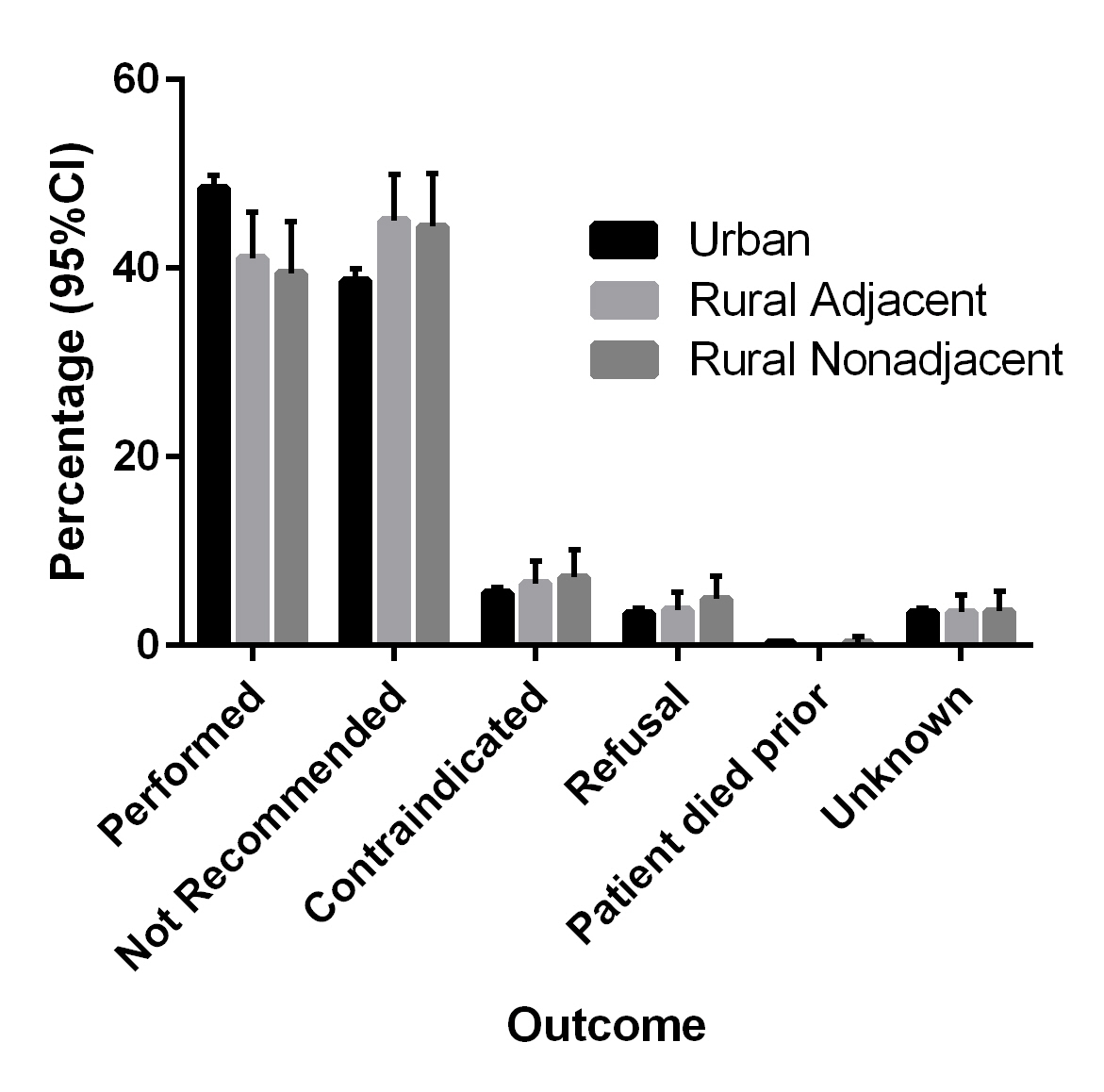
Figure 1: Surgical decisionmaking for Stage I Pancreas Cancer by County Characteristics
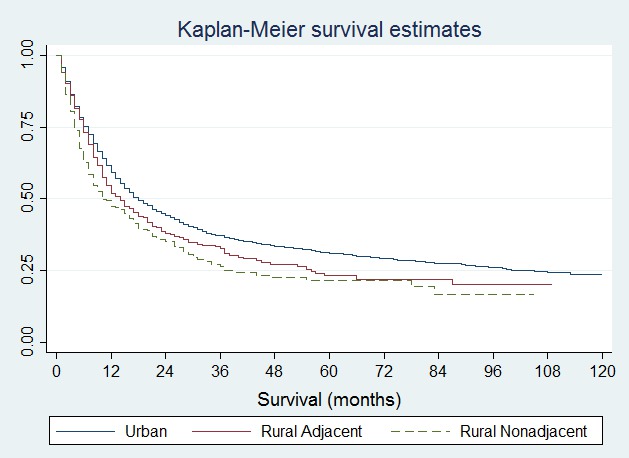
Figure 2: Survival by County of Residence for Stage I pancreas cancer
Back to 2017 Posters
|