|
Back to 2017 Posters
SIZE OF PANCREATIC NEUROENDOCRINE TUMORS CORRELATES WITH RISK OF LYMPH NODE METASTASIS
Theodoros Michelakos*1, Giovanni Marchegiani2, Carlos Fernandez-Del Castillo1, Kim C. Honselmann1, Lei Cai1, Marco Miotto2, Luca Landoni2, Andrew L. Warshaw1, Keith D Lillemoe1, Claudio Bassi2, Cristina R. Ferrone1
1Massachusetts General Hospital, Boston, MA; 2Verona University Hospital, Verona, Italy
Background: Lymph node (LN) dissection for pancreatic neuroendocrine tumors (PNETs) has been heavily debated over the years. The aim of this collaborative effort was to assess the incidence of positive lymph nodes in PNETs <4cm and to determine if there was a difference between functional and non-functional PNETs.
Methods: Clinicopathologic factors of PNETs operated on at a high volume US and European center between 1998-2015 were collected and combined in a single database.
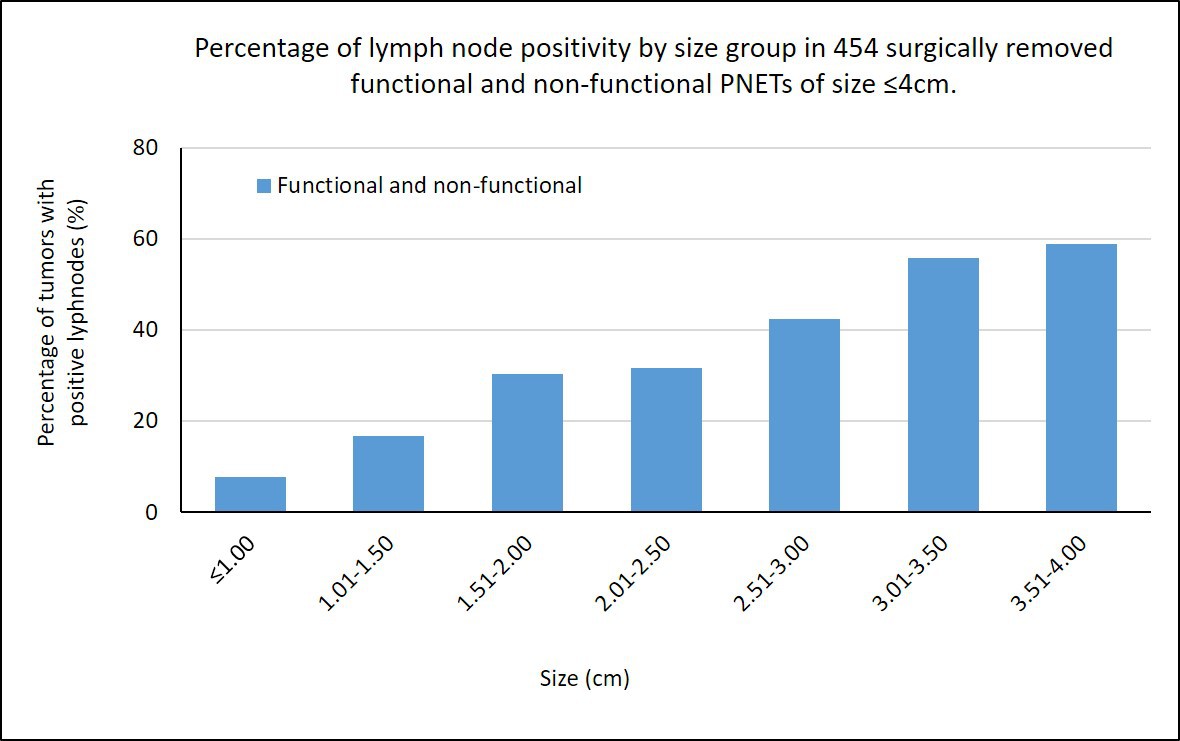
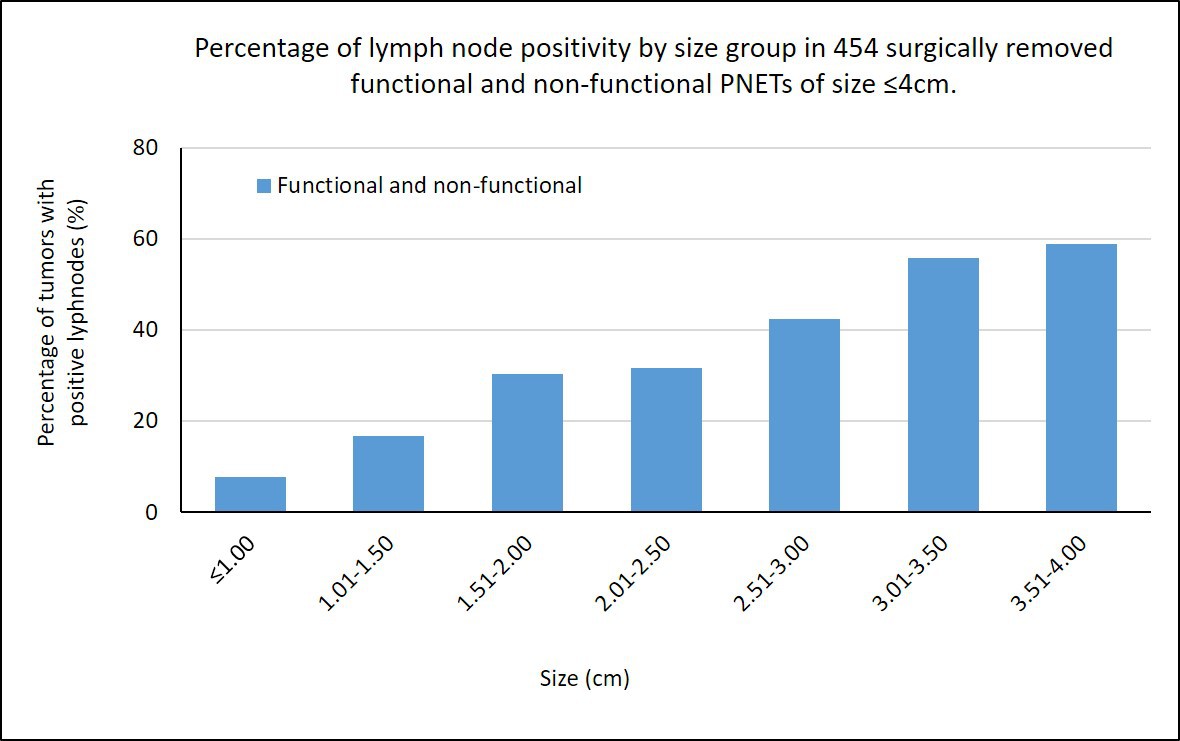
Results: A total of 617 patients were resected, of whom 454 (74%) PNETs were ≤4cm. The majority (78%, 355/454) had non-functional tumors. Patients with non-functional PNETs were older (55 vs. 51y; p=0.04), had larger tumors (2 vs. 1.5cm; p<0.001) and higher WHO grade (grades 1 [65% vs. 84%], 2 [30% vs. 15%], 3 [4% vs. 1%]; p=0.003). Increasing rate of lymph node positivity correlated with increasing size of the PNET (p<0.001) (Figure). Frequency of positive LNs was higher among non-functional PNETs overall (33% vs 19%; p=0.01), but the association was lost within size groups. Patients with positive LNs had a worse overall survival (p<0.001). The ROC curve demonstrated that a cutoff value of 2cm predicts LN+ with sensitivity and specificity of 72% and 67%, respectively (AUC: 0.711; p<0.001).
Conclusion: As PNET size increases, the risk of LN positivity increases. Based on the ROC curve, patients with tumor sizes ≥2cm would benefit from a LN dissection at the time of the operation.
Back to 2017 Posters
|